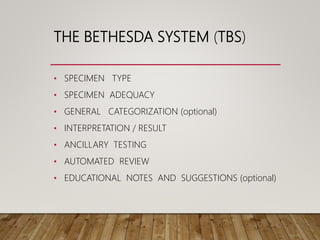
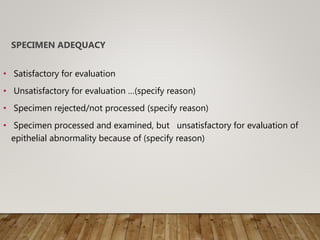
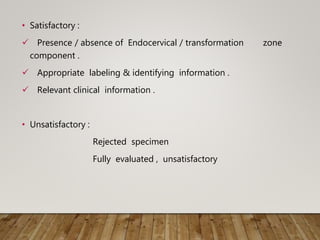
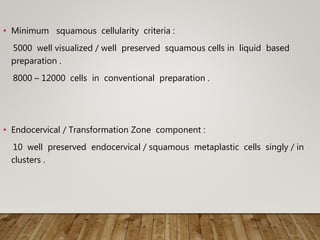
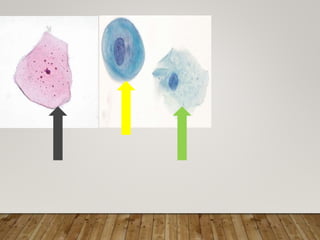
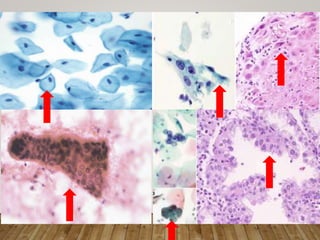
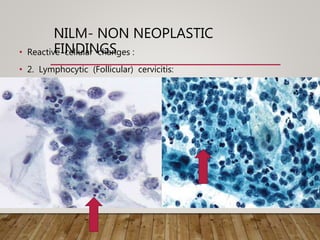
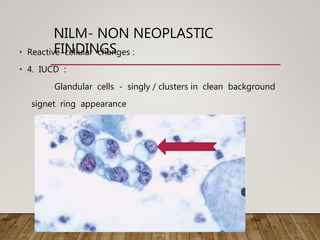
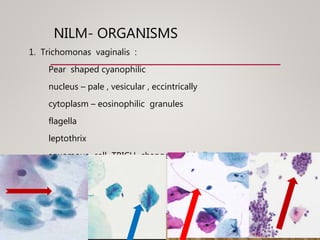
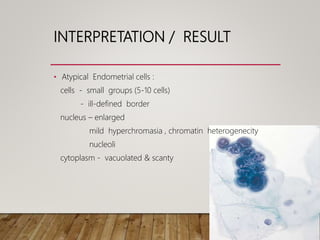
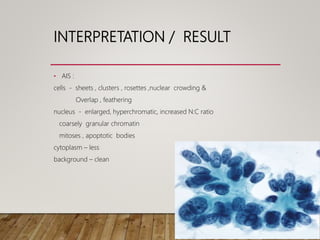
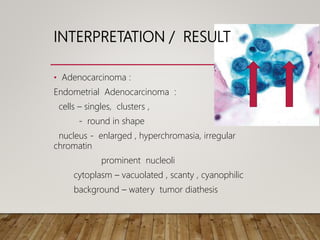
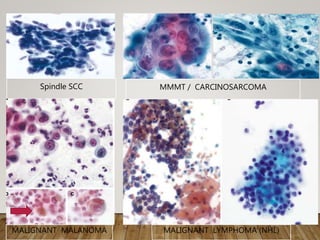
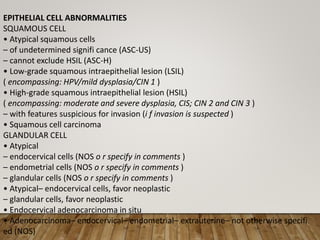
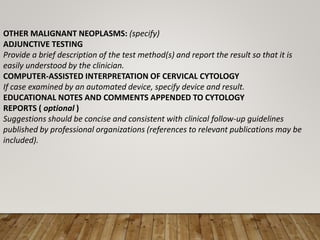
The Bethesda System is a standardized reporting system used for Pap test results. It provides a structured format for reporting cervical and vaginal cytology diagnoses. The system includes sections for specimen type, adequacy, interpretation/result, and optional notes. Interpretation/result categories include negative for intraepithelial lesion or malignancy, epithelial cell abnormalities (such as atypical squamous cells, low-grade squamous intraepithelial lesion, or high-grade squamous intraepithelial lesion), and other malignant neoplasms. Specific cytological features are described for each category. The system aims to improve consistency and communication of Pap test results.