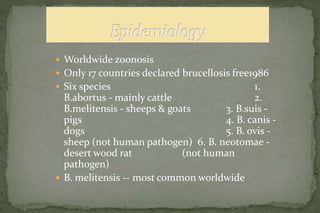
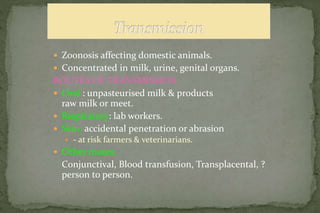
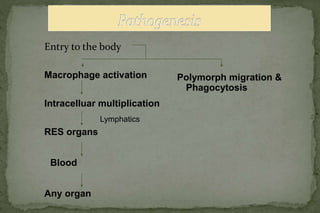
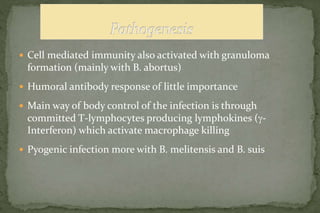
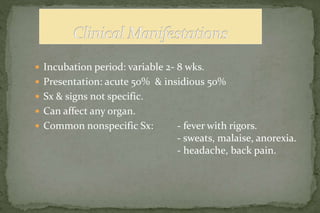
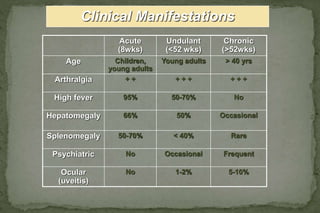
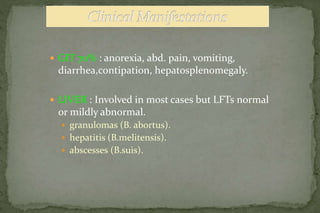
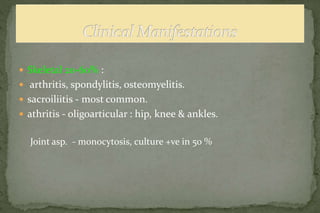
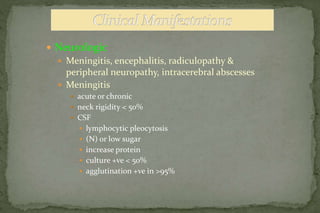
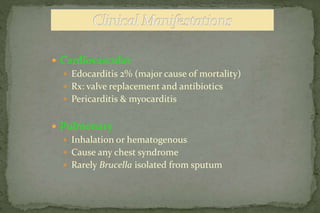
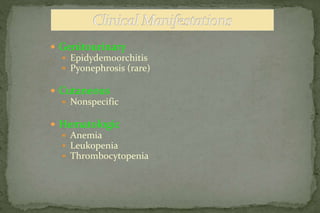
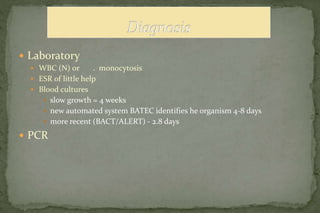
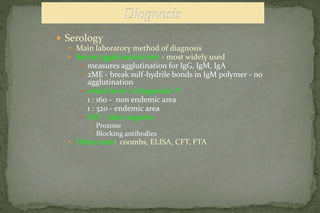
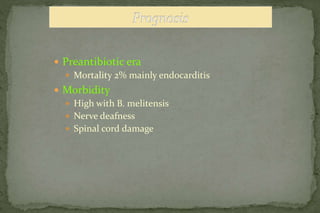
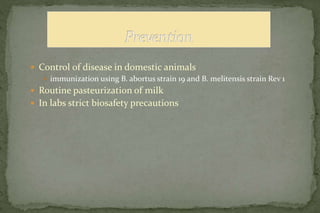
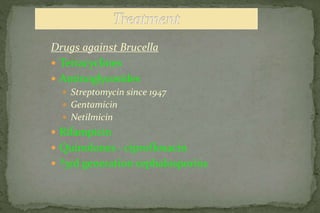
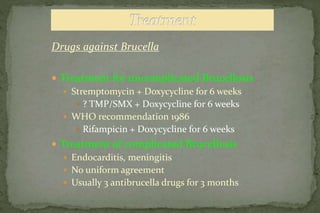
This document discusses Brucellosis, a zoonotic disease caused by bacteria from the Brucella genus. It notes that Brucellosis is endemic in many parts of the world, with six main species that can infect different animal hosts. The most common cause of human infection is B. melitensis from goats and sheep. Transmission occurs through contact with infected animals or consumption of unpasteurized dairy. Clinical presentation in humans is non-specific with fever being the most common symptom. Diagnosis involves blood cultures, serology or PCR. Treatment consists of a combination of doxycycline and rifampin or streptomycin for 6 weeks. Control relies on vaccination of livestock and pasteurization