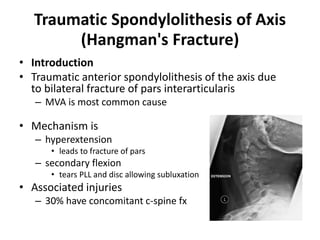
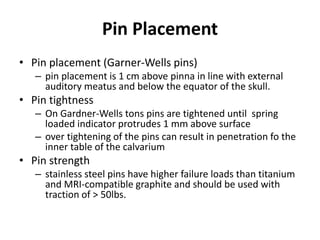
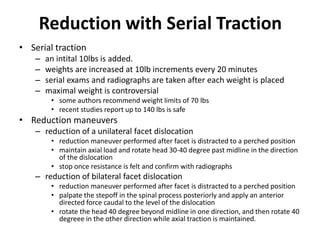
This document discusses cervical spine injuries and their classification, as well as treatments for cervical trauma including cervical traction and halo orthosis immobilization. It separates cervical injuries into upper cervical injuries from the skull base to C2, and sub-axial injuries from C3 to C7. It provides details on traction techniques and halo application, indicating they are effective non-surgical treatments for fractures like hangman's fractures and stable fractures. Complications of traction and halo use include failure to reduce, neurological changes, loosening, infection and nerve palsies.