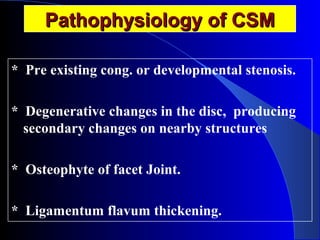
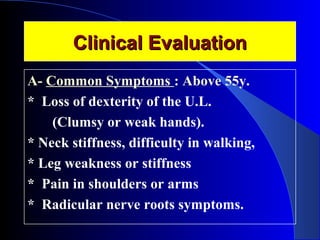
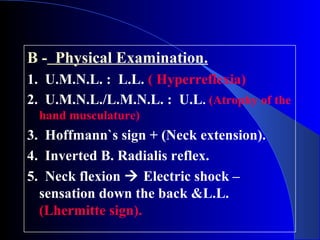
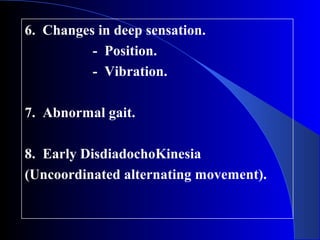
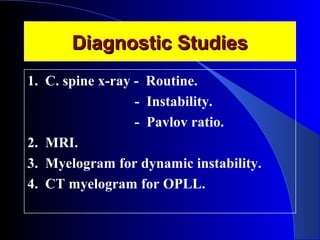
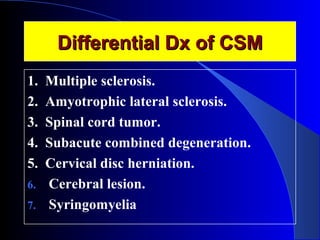
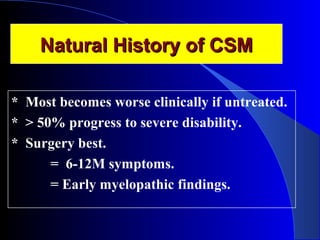
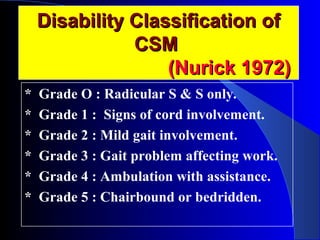
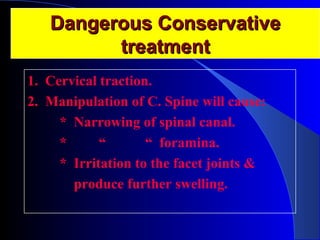
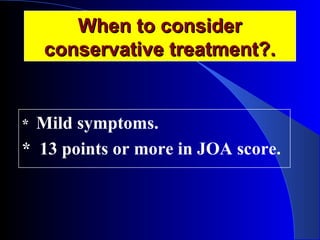
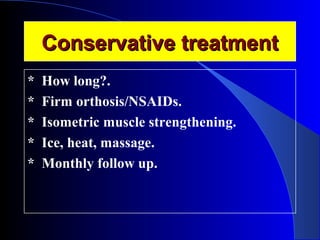
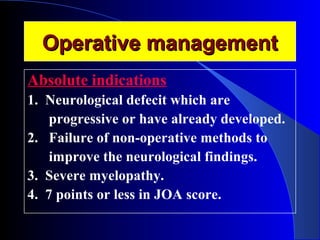
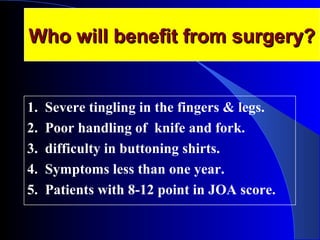
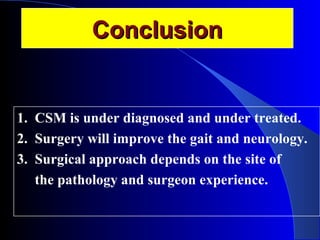
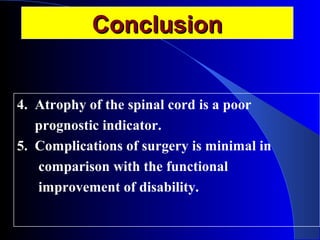
Cervical Myelopathy (CSM) is a common spinal cord dysfunction often seen in individuals over 55, characterized by symptoms such as loss of dexterity, neck stiffness, and leg weakness. Diagnosis involves clinical evaluation and imaging studies, while treatment options range from conservative management to surgical intervention, depending on symptom severity and progression. The document emphasizes the importance of recognizing and treating CSM early to improve patient outcomes and decrease the risk of severe disability.