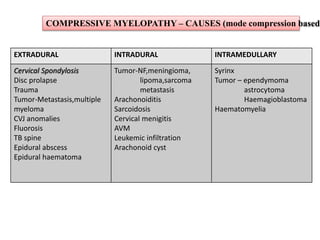
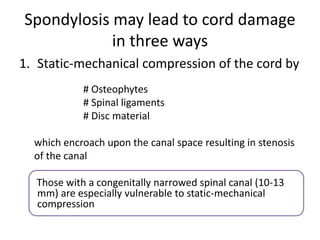
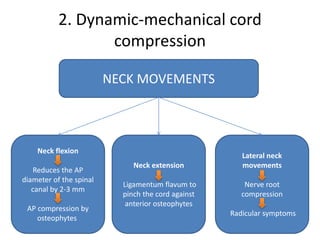
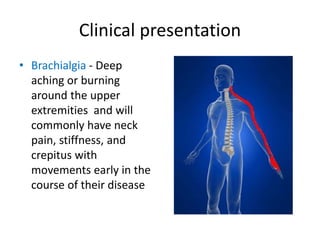
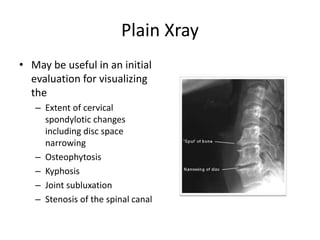
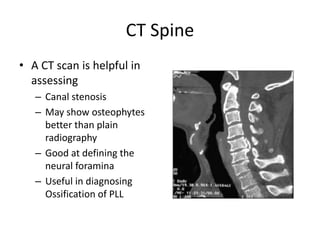
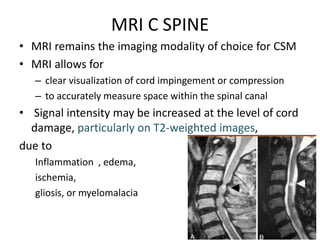
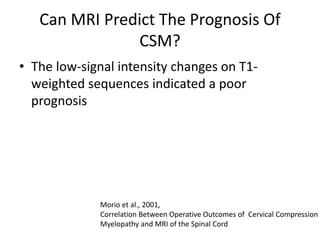
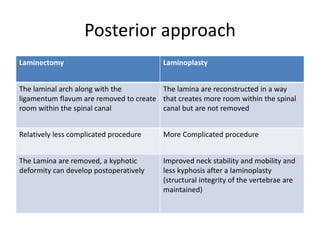
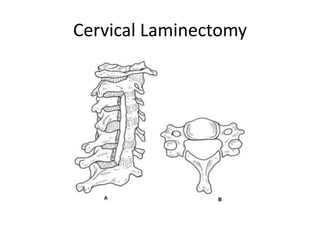
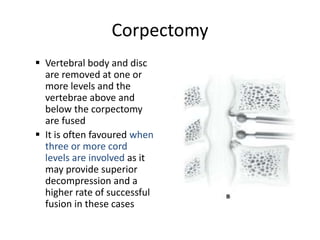
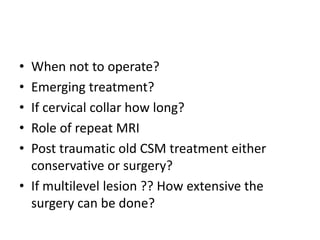
Cervical spondylotic myelopathy (CSM) is the most common cause of spinal cord dysfunction in older adults, occurring when cervical spine degeneration compresses the spinal cord. Common symptoms include neck pain, numbness, and weakness. MRI is the preferred imaging test to evaluate cord compression and signal changes. Treatment options include cervical collars, medications for pain relief, and surgery. Surgery involves decompressing the spinal cord through either an anterior or posterior approach, and often spinal fusion is also needed for stability. Earlier surgery and less preoperative cord signal changes on MRI predict better surgical outcomes.