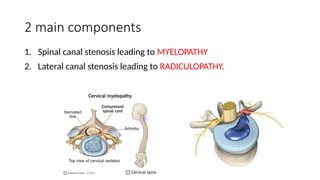
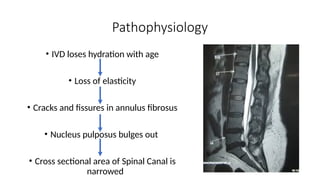
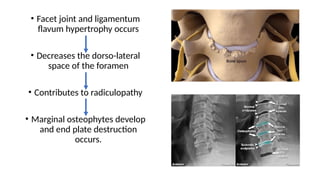
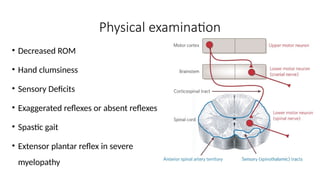
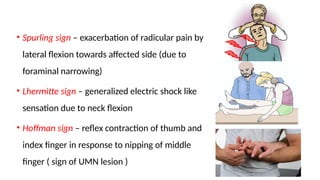
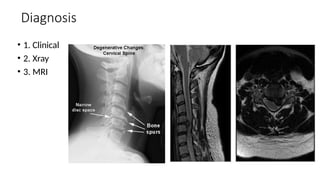
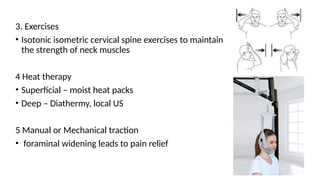
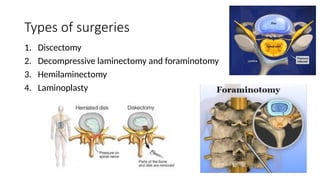
Cervical spondylosis is a chronic degenerative disorder of the cervical spine that typically affects individuals over 40 years old, resulting from normal aging processes, including the deterioration of vertebrae, discs, and ligaments. Common symptoms include chronic neck pain, radiculopathy, and potentially severe cervical spondylotic myelopathy, which can lead to significant neurological deficits. Treatment options range from conservative management, such as immobilization and physical therapy, to surgical interventions for severe cases.