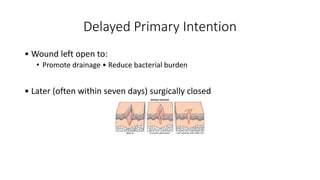
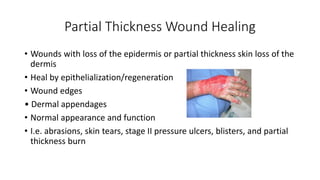
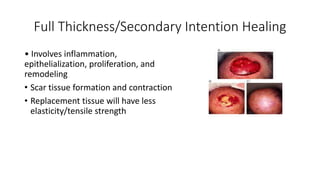
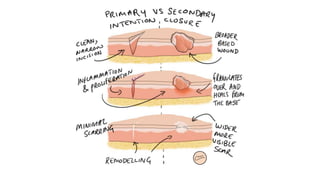
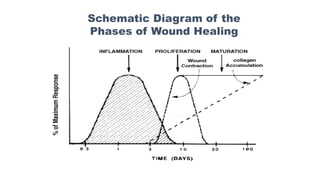
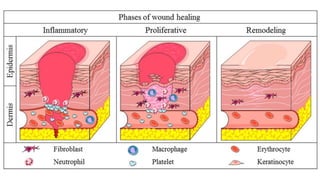
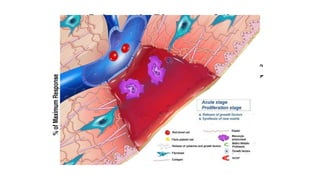
Wound healing involves a cascade of biological events that results in a closed wound. There are different types of wound healing depending on the depth and severity of the wound. The normal wound healing process consists of three main phases - inflammation, proliferation, and remodeling. Many factors can affect wound healing including the characteristics of the wound and patient as well as how the wound is managed and dressed. Proper wound assessment and choosing the right dressing are important for optimizing the healing process.