The document discusses portal hypertension, including:
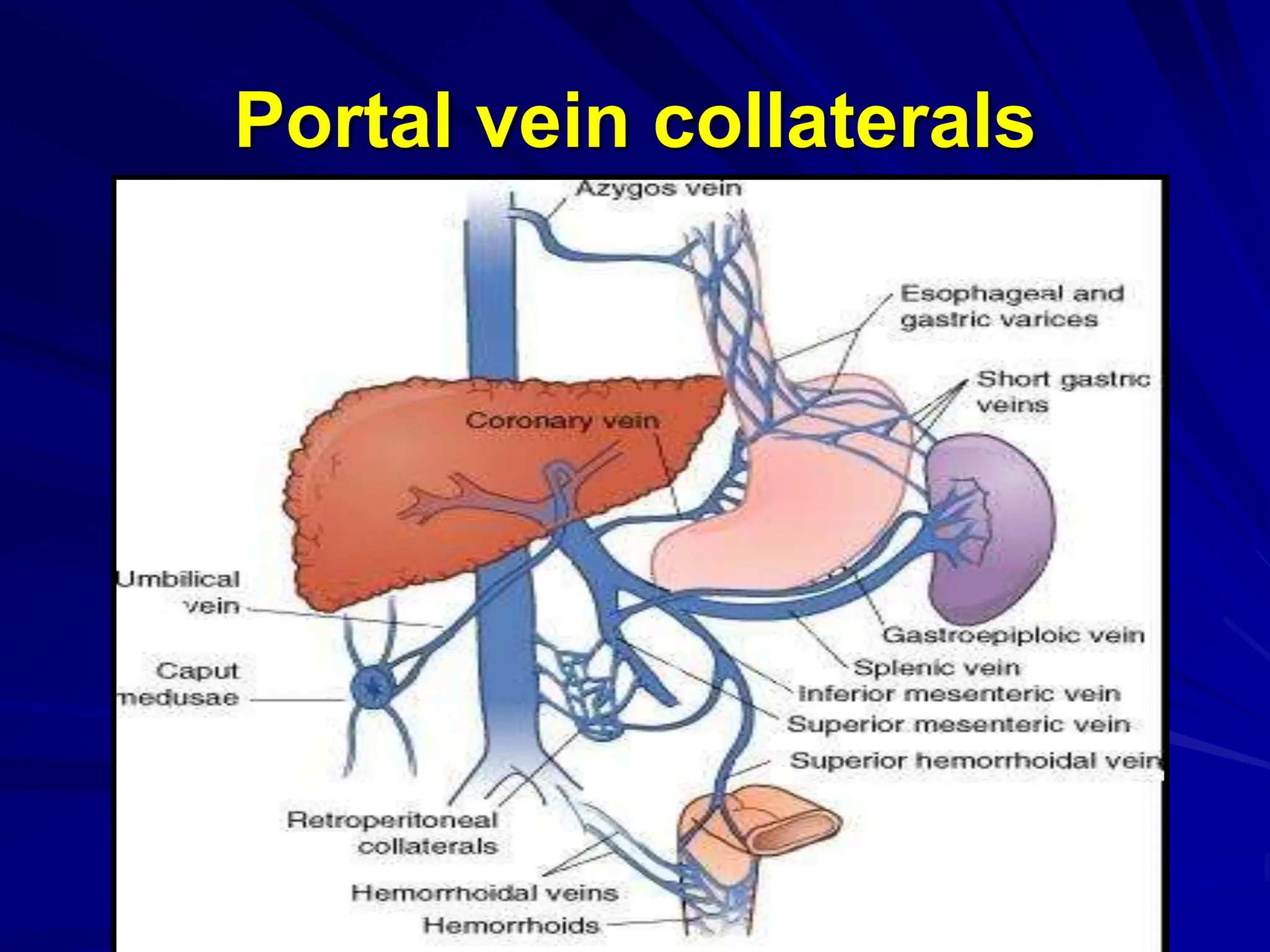
- Anatomy of the portal vein and causes of increased portal pressure.
- Cirrhosis of the liver is a leading cause of portal hypertension due to obstruction of blood flow through the liver.
- Consequences of portal hypertension include splenomegaly, variceal bleeding, and ascites.
- Investigations involve assessing liver function and imaging tests to identify varices.
- Treatment depends on severity but may include band ligation, sclerotherapy, drugs, or shunt surgery to reduce portal pressure.