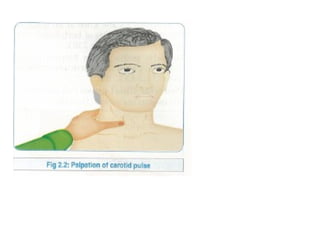
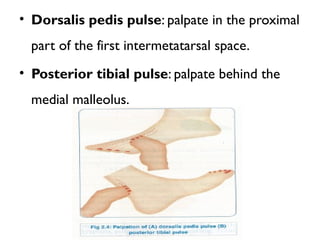
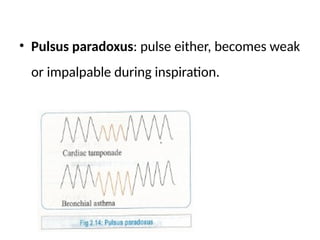
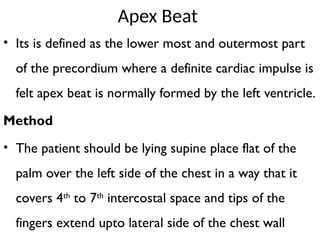
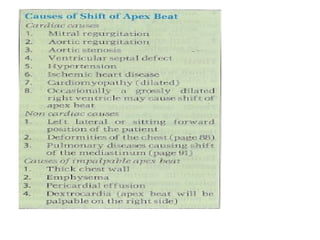
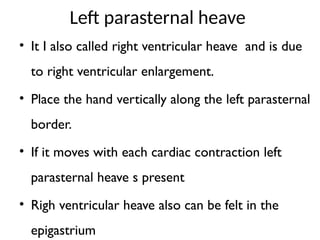
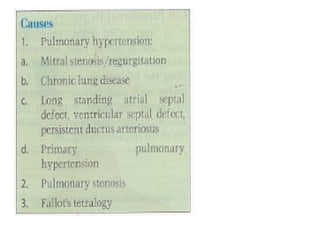
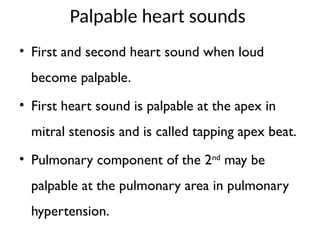
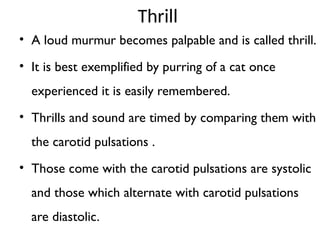
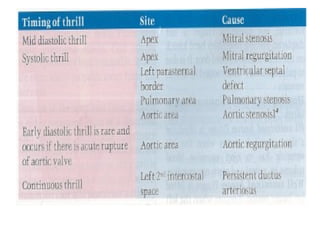
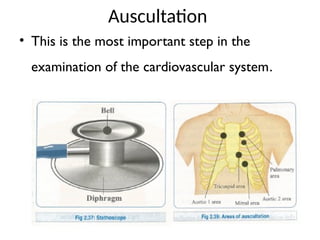
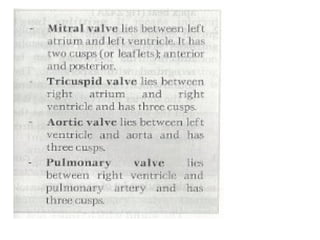
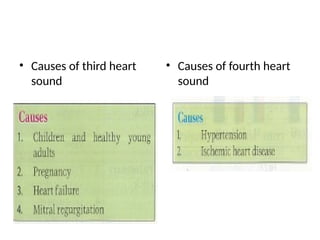
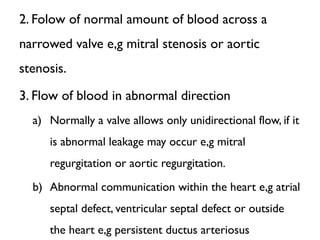
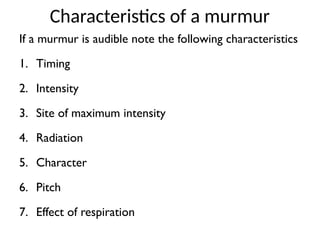
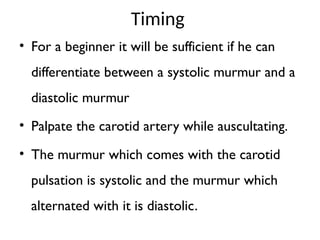
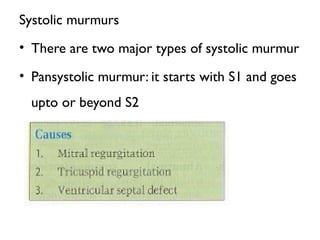
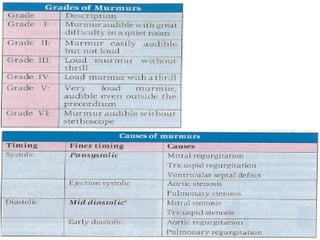
This document details the cardiovascular physical examination, highlighting the importance of clinical assessment for accurate diagnosis of cardiovascular diseases. It discusses key symptoms such as dyspnea and chest pain, along with their characteristics, and provides an extensive guide on how to conduct a thorough cardiovascular examination, including pulse assessment, neck vein inspection, and precordial examination techniques. Additionally, it covers heart sounds, murmurs, and their significance in diagnosing heart conditions.