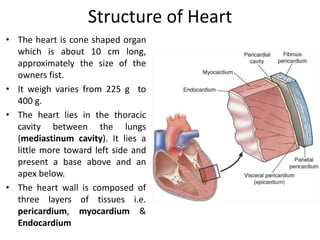
The cardiovascular system consists of the heart and blood vessels. The heart pumps blood through a network of arteries, capillaries and veins. The heart has four chambers and is composed of three layers. It is located in the chest cavity slightly left of center. The heart's natural pacemaker, the sinoatrial node, initiates electrical impulses that cause coordinated contractions. Blood pressure, cardiac output and peripheral resistance determine blood flow. Diseases can disrupt blood flow and oxygen delivery, like atherosclerosis, heart failure and ischemic heart disease including angina and myocardial infarction.