The document discusses cardiovascular physiology, including:
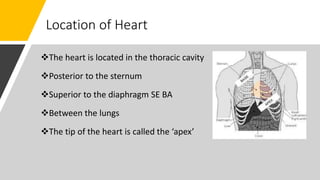
- The location of the heart in the thoracic cavity between the lungs.
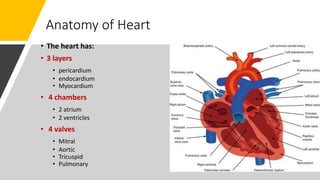
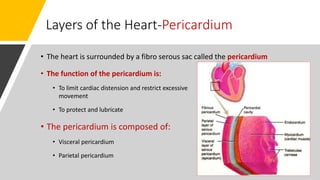
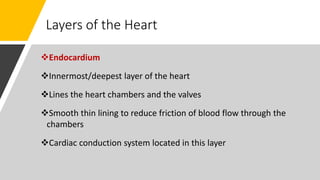
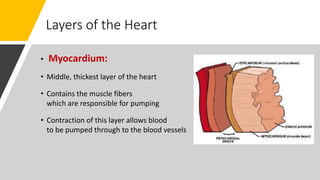
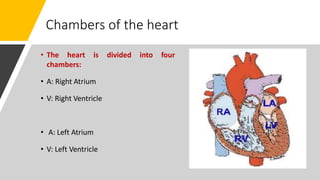
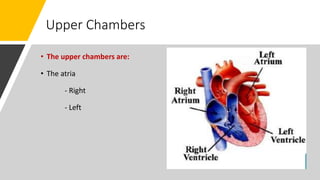
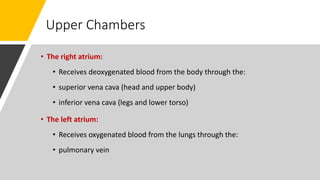
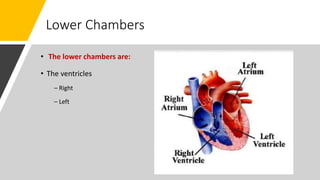
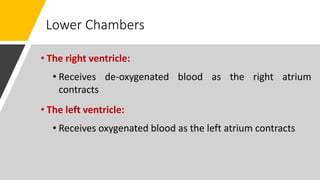
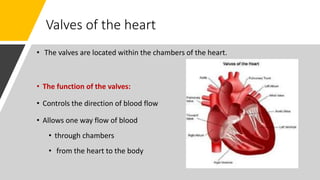
- The three layers of the heart - pericardium, endocardium, and myocardium - and its four chambers - two atria and two ventricles.
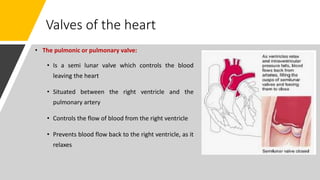
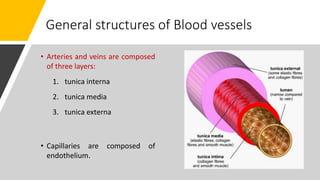
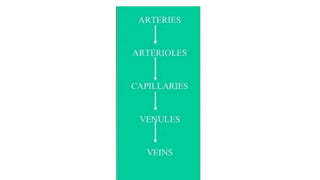
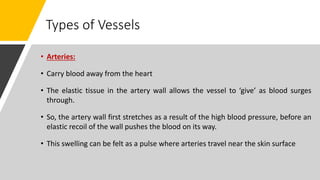
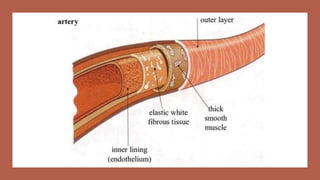
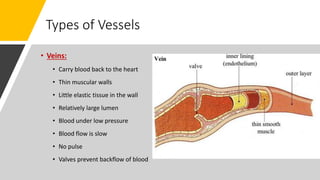
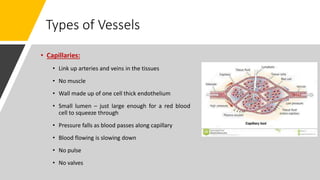
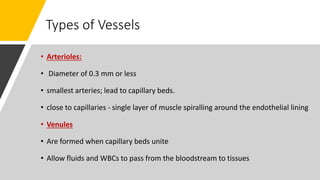
- The heart pumps oxygenated blood to the body and deoxygenated blood returns to the heart through arteries, veins and capillaries.
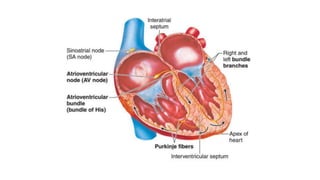
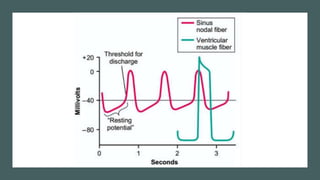
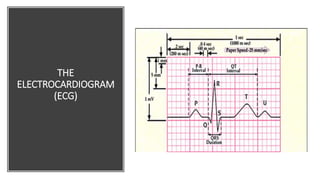
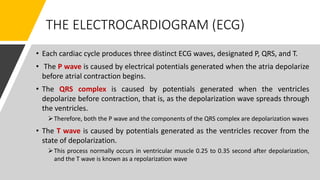
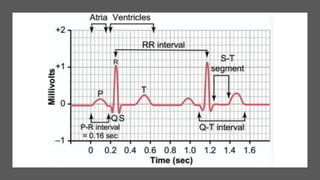
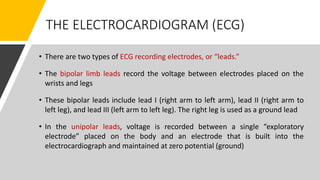
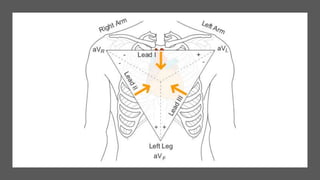
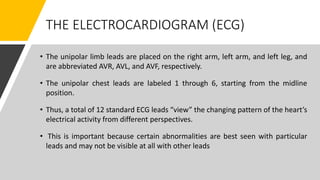
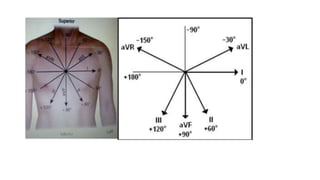
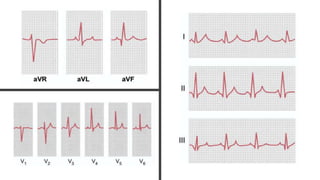
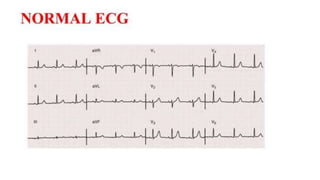
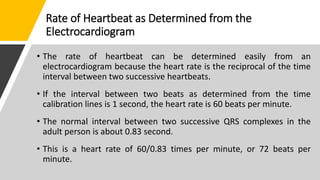
- The electrical conduction system generates heartbeats and the electrocardiogram can be used to measure heart rate and rhythm.