The document summarizes the cardiovascular system, including:
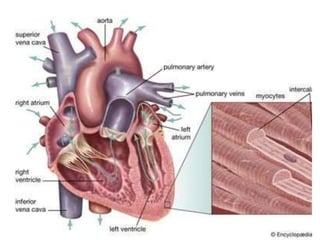
1. The anatomy and physiology of the heart, including its chambers and layers. The heart pumps deoxygenated blood to the lungs and oxygenated blood to the body.
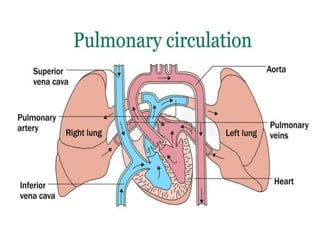
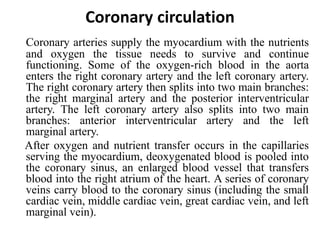
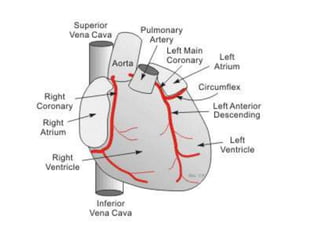
2. The three main types of blood circulation - pulmonary circulation between the heart and lungs, coronary circulation supplying the heart, and systemic circulation supplying the body. Blood vessels have three layers and blood flows through arteries, arterioles, capillaries and veins.
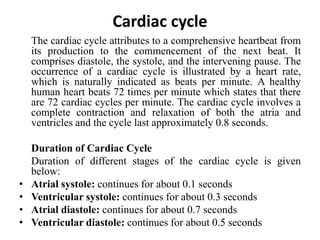
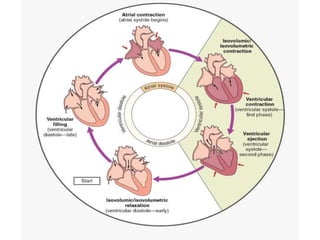
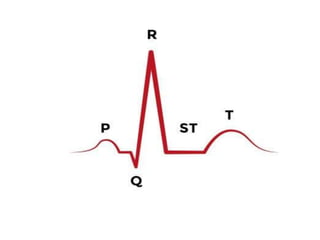
3. Key aspects of cardiac cycle including the phases of atrial and ventricular systole and diastole. Heart sounds and electrocardiograms are also summarized.