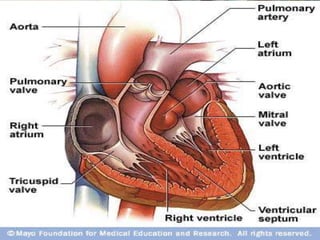
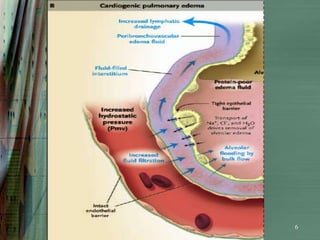
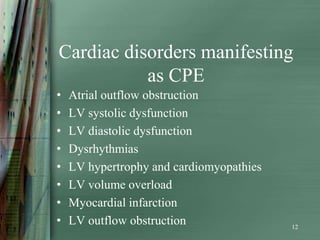
1) Cardiogenic pulmonary edema (CPE) occurs when increased hydrostatic pressure in the pulmonary capillaries causes fluid to leak into the lungs due to left ventricular dysfunction or elevated left atrial pressure.
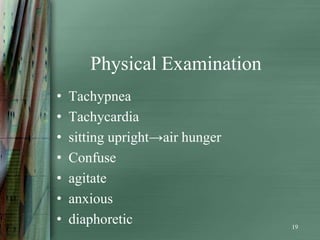
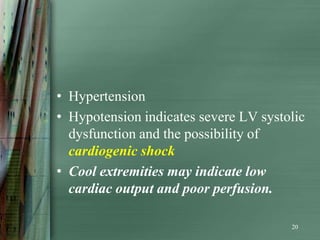
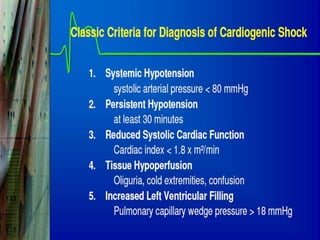
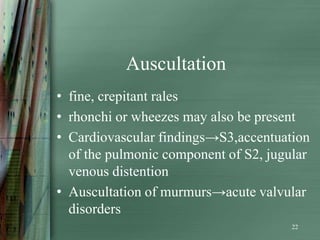
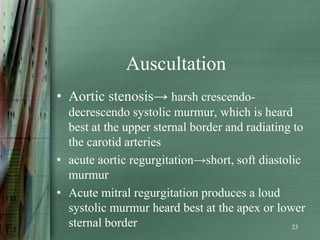
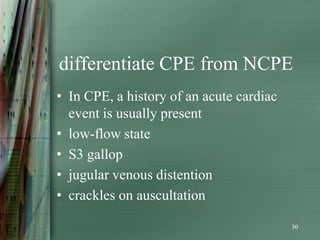
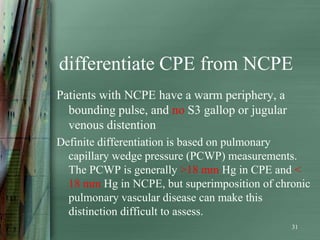
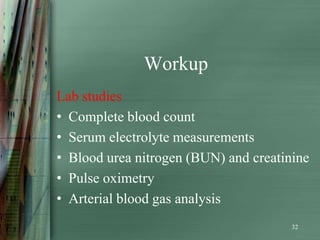
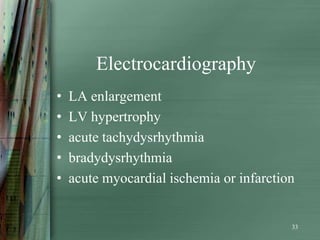
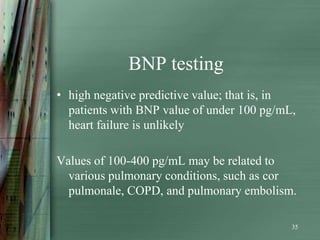
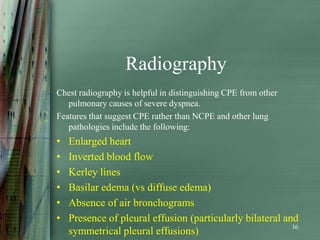
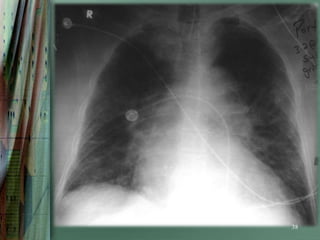
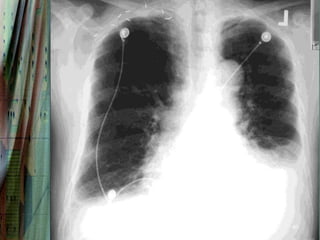
2) Diagnosis is based on history, physical exam findings of tachypnea, tachycardia, crackles on auscultation, and tests like chest x-ray, EKG, BNP, echocardiogram and pulmonary artery catheter.
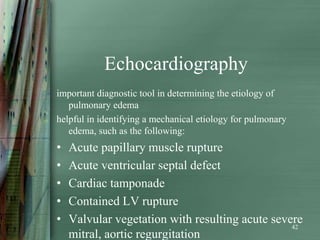
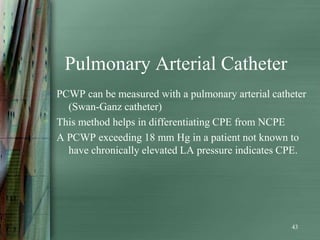
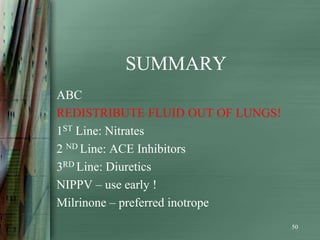
3) Treatment focuses on reducing preload and afterload through medications like nitrates, ACE inhibitors, diuretics and vasodilators, as well as providing supportive care through oxygen, ventilation if needed, and inotro