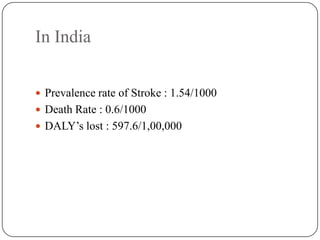
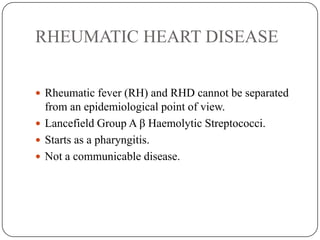
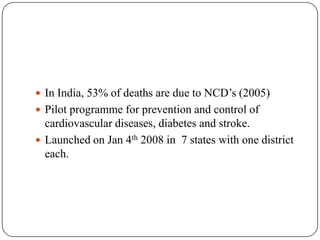
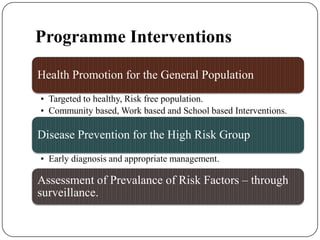
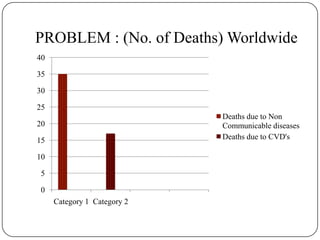
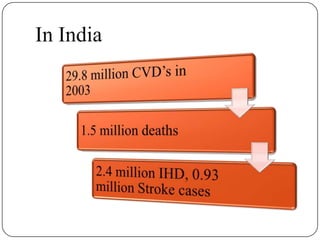
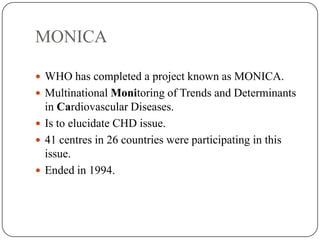
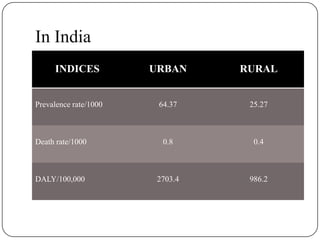
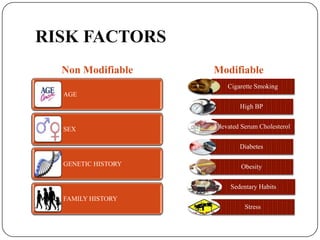
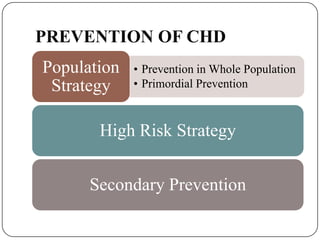
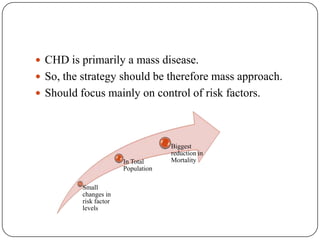
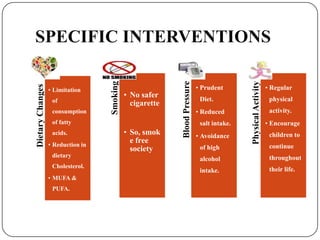
Cardiovascular diseases (CVDs) are a group of conditions that affect the heart and blood vessels. The major CVDs are ischemic heart disease, hypertension, stroke, congenital heart disease, and rheumatic heart disease. Worldwide, CVDs are the leading cause of deaths, responsible for over 30 million deaths annually. In India, the prevalence of coronary heart disease is higher in urban versus rural areas. Some key risk factors for CVDs include age, family history, smoking, high blood pressure, high cholesterol, diabetes, and physical inactivity. Prevention strategies target populations through risk factor modification as well as high-risk individuals through screening and management. The WHO has implemented projects like MONICA to study CVD trends and determin
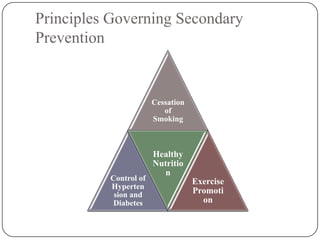
![ Forms an important part of an overall strategy.
Aim is to prevent the recurrence and progression of
CHD.
Rapidly expanding field with much of research in
progress. [ E.g. drug trials, coronary surgery, pace
makers ]](https://image.slidesharecdn.com/cardiovasculardiseases-131009102041-phpapp01/85/Cardio-vascular-diseases-19-320.jpg)