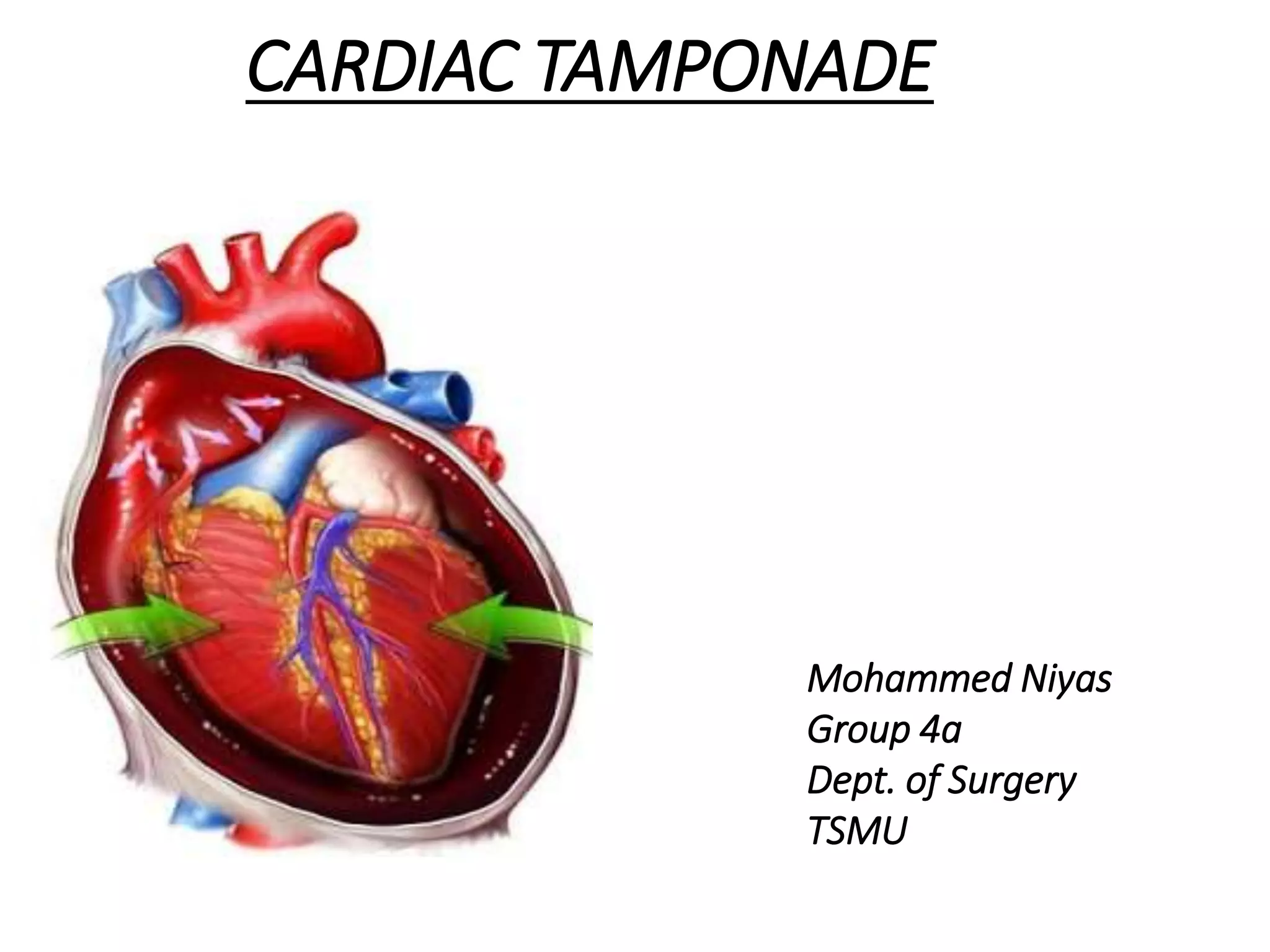
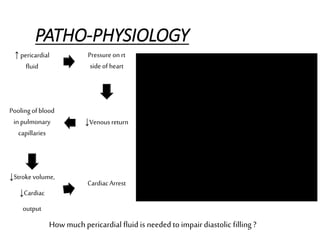
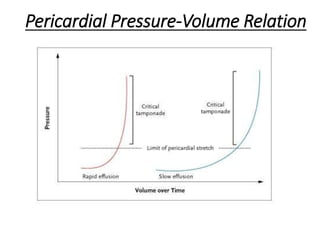
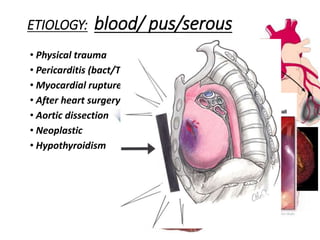
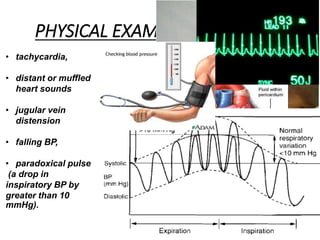
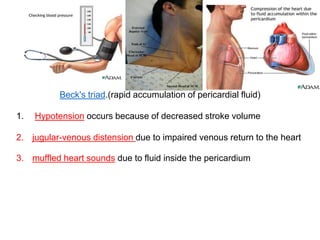
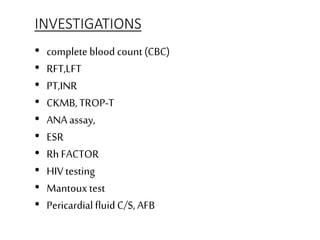
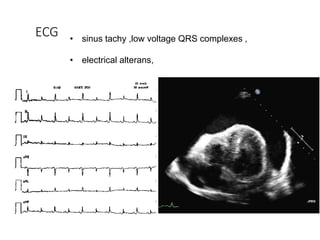
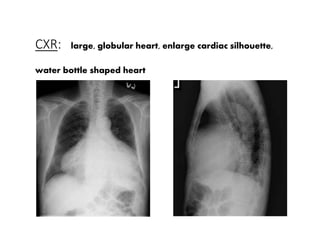
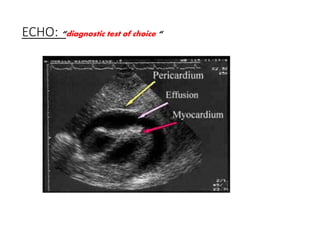
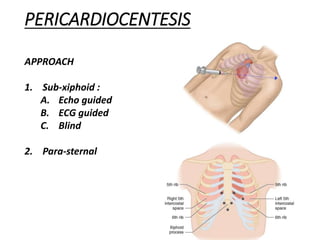
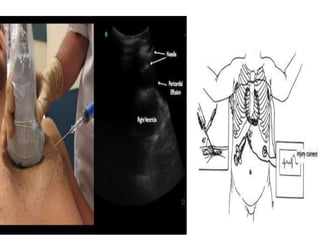
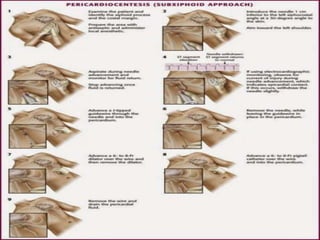
Cardiac tamponade is a medical emergency caused by an accumulation of fluid in the pericardial space, which surrounds the heart. This increased fluid pressure restricts the heart's filling and reduces cardiac output. If untreated, cardiac tamponade is rapidly fatal. Diagnosis is made through physical exam findings, electrocardiogram, chest x-ray and echocardiogram. Pericardiocentesis, a procedure to drain the fluid via needle insertion, provides immediate relief and is lifesaving for cardiac tamponade. After the procedure, close monitoring is needed to watch for potential complications and recurrence of fluid buildup.