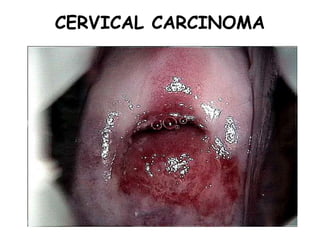
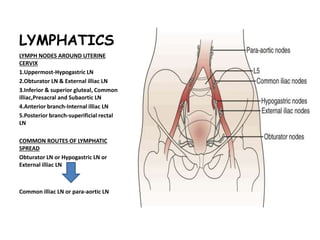
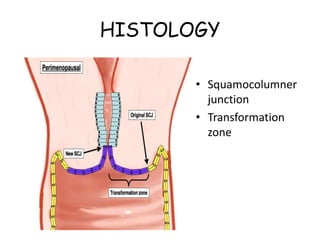
1. Cervical carcinoma arises from the cervix which has lymphatic drainage to the hypogastric, obturator, external iliac, and common iliac lymph nodes.
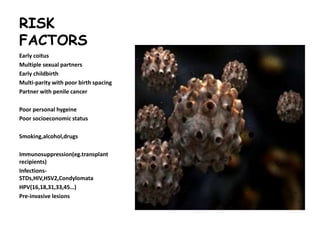
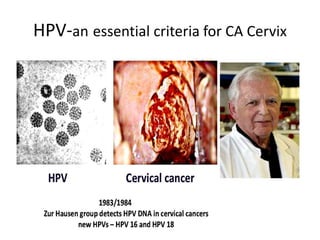
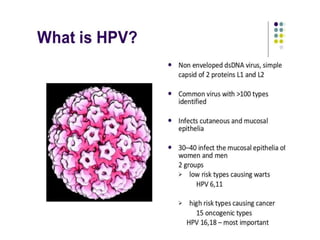
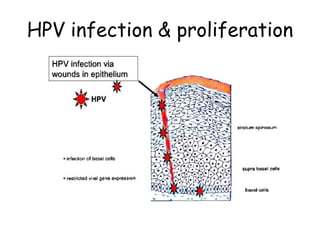
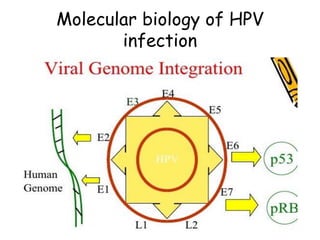
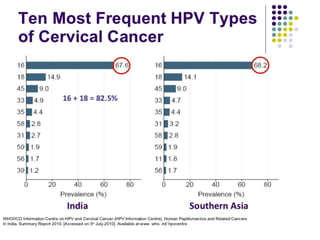
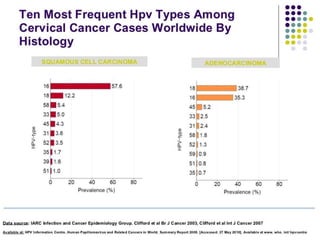
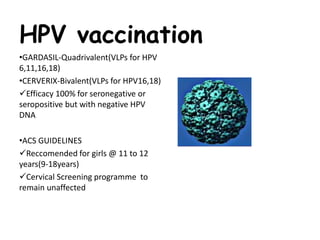
2. Risk factors include early age of first intercourse, multiple sexual partners, HPV infection, smoking, and poor socioeconomic status.
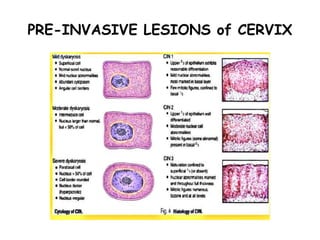
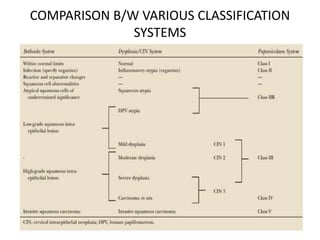
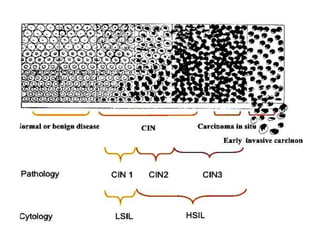
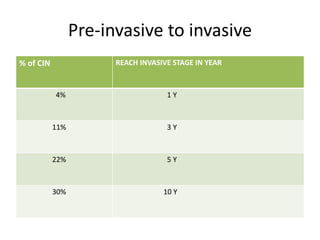
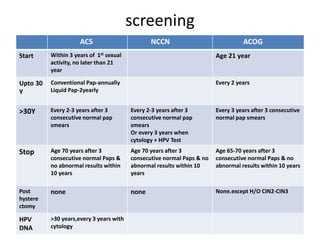
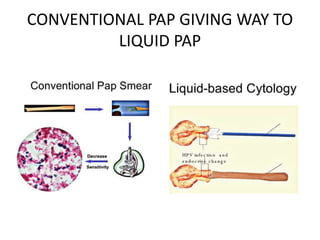
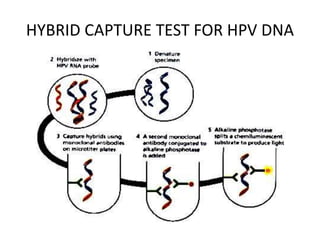
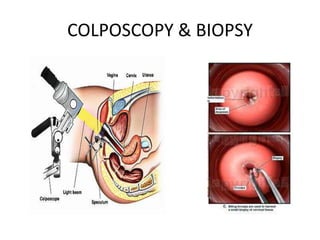
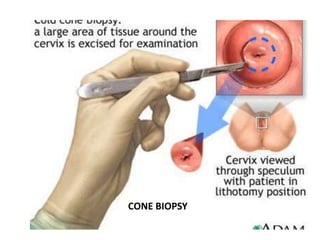
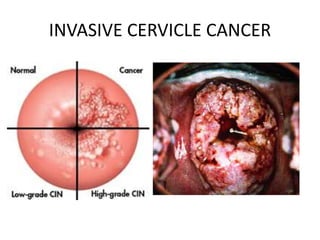
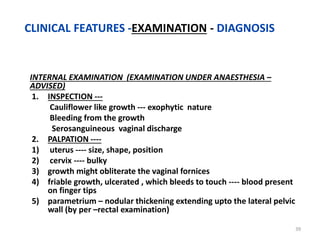
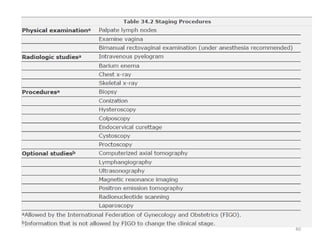
3. Screening involves Pap smear testing which is transitioning to liquid based cytology and HPV testing. Colposcopy and biopsy are used for diagnosis.
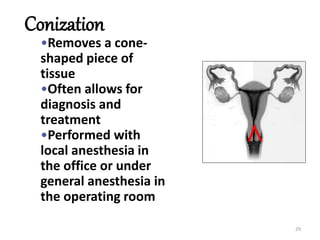
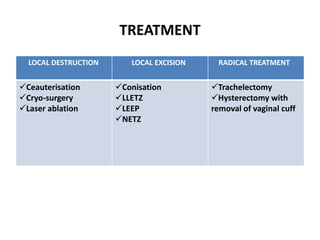
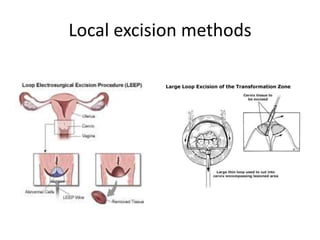
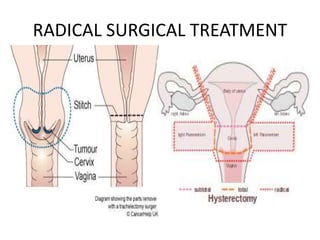
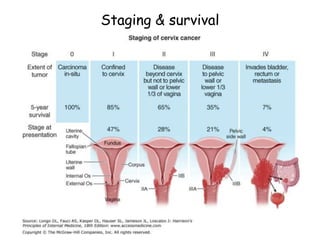
4. Treatment ranges from local destruction for pre-invasive lesions to radical surgery or chemoradiation for invasive cancer, depending on the stage.