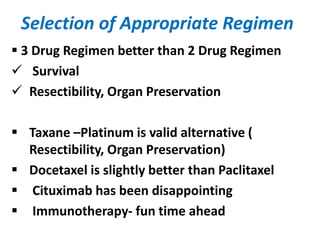
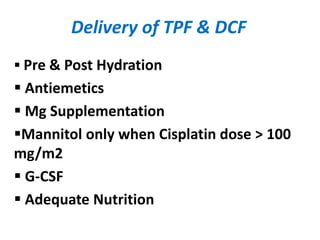
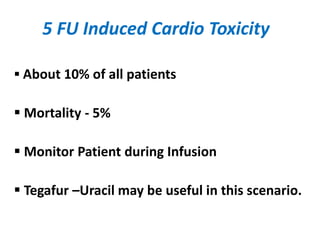
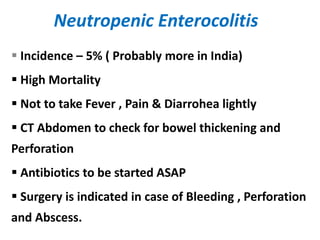
This document summarizes key points from an NACT workshop. It discusses how NACT can improve outcomes for locally advanced nasopharyngeal carcinoma and help preserve organs for cancers of the hypopharynx, larynx, and oral cavity. The document also covers appropriate patient selection, choosing effective NACT regimens, managing toxicities like neutropenic enterocolitis, assessing patient response to NACT, surgery after NACT, and managing radiation therapy after NACT. The overall goals of NACT are to improve survival, make tumors more operable, and help preserve organs and functions.