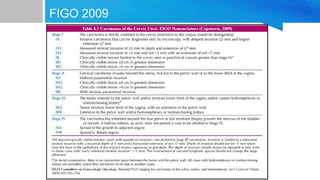
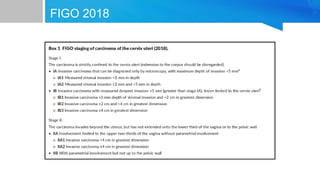
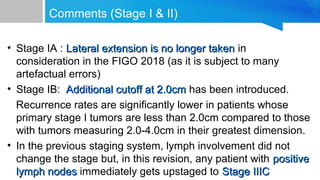
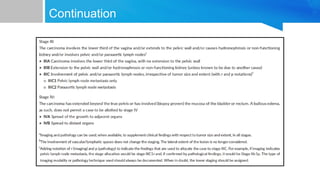
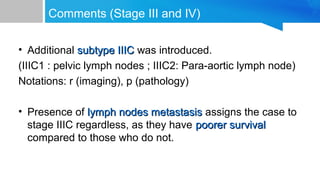
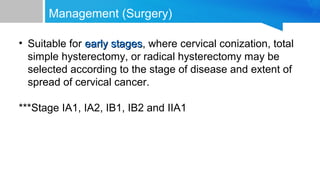
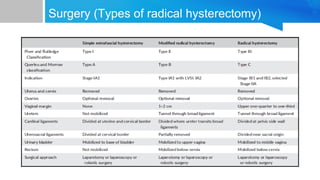
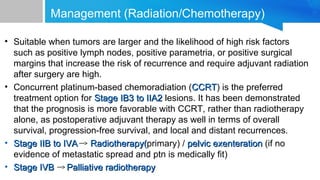
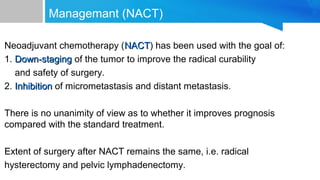
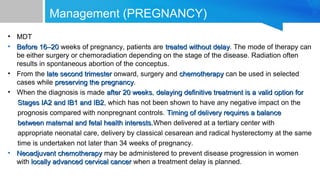
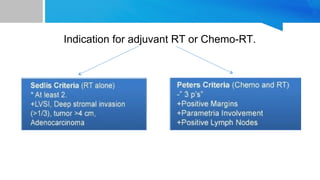
The FIGO classification for cervical cancer was revised in 2018 to incorporate imaging and pathological findings to better determine tumor size and extent of disease. Key changes include upstaging any cancer with lymph node involvement to Stage IIIc and introducing a new cutoff of 2cm for Stage Ib cancers. Surgery is recommended for early stages while concurrent chemoradiation is preferred for Stage Ib3 to IIa2 lesions. Later stages receive primary radiotherapy or chemoradiation with surgery an option for select Stage IIb to Iva cases. Neoadjuvant chemotherapy may help downstage tumors but does not clearly improve prognosis. Pregnancy does not alter treatment approach before 16-20 weeks but chemotherapy and delayed surgery are options after that