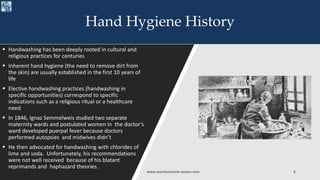
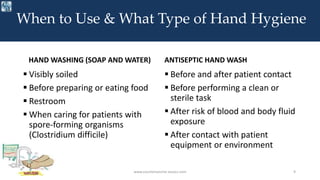
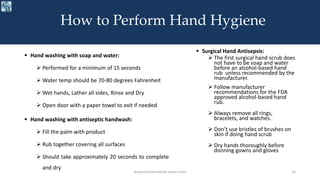
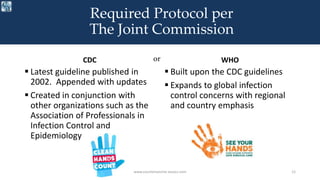
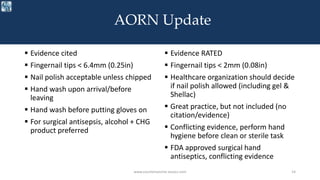
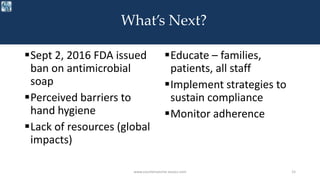
The document discusses hand hygiene history, guidelines, and standards. It compares the CDC and WHO hand hygiene guidelines and examines updates to the AORN hand hygiene standards. The CDC established guidelines in 2002 and the WHO built upon these to be more applicable globally. The AORN recently updated standards on nail length, polish, hand washing/rub timing and products. Going forward, adherence will need to be monitored and strategies implemented to sustain compliance with hand hygiene practices.