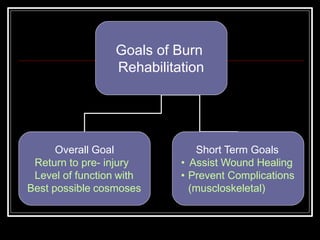
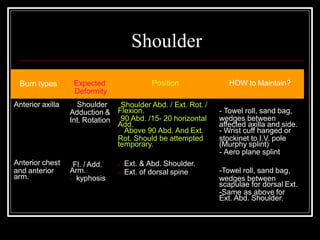
The document discusses goals and techniques for burn rehabilitation. The overall goal is to return patients to their pre-injury level of function with the best possible cosmetic outcome. Short term goals include assisting wound healing and preventing complications. Key techniques discussed include positioning, splinting, and electrotherapeutic modalities to aid healing and prevent contractures. Positioning aims to maintain burned tissues in an elongated state using various supports. Splinting provides support and helps maintain joint positions. Modalities like ultrasound, laser, and UV radiation can accelerate healing processes.