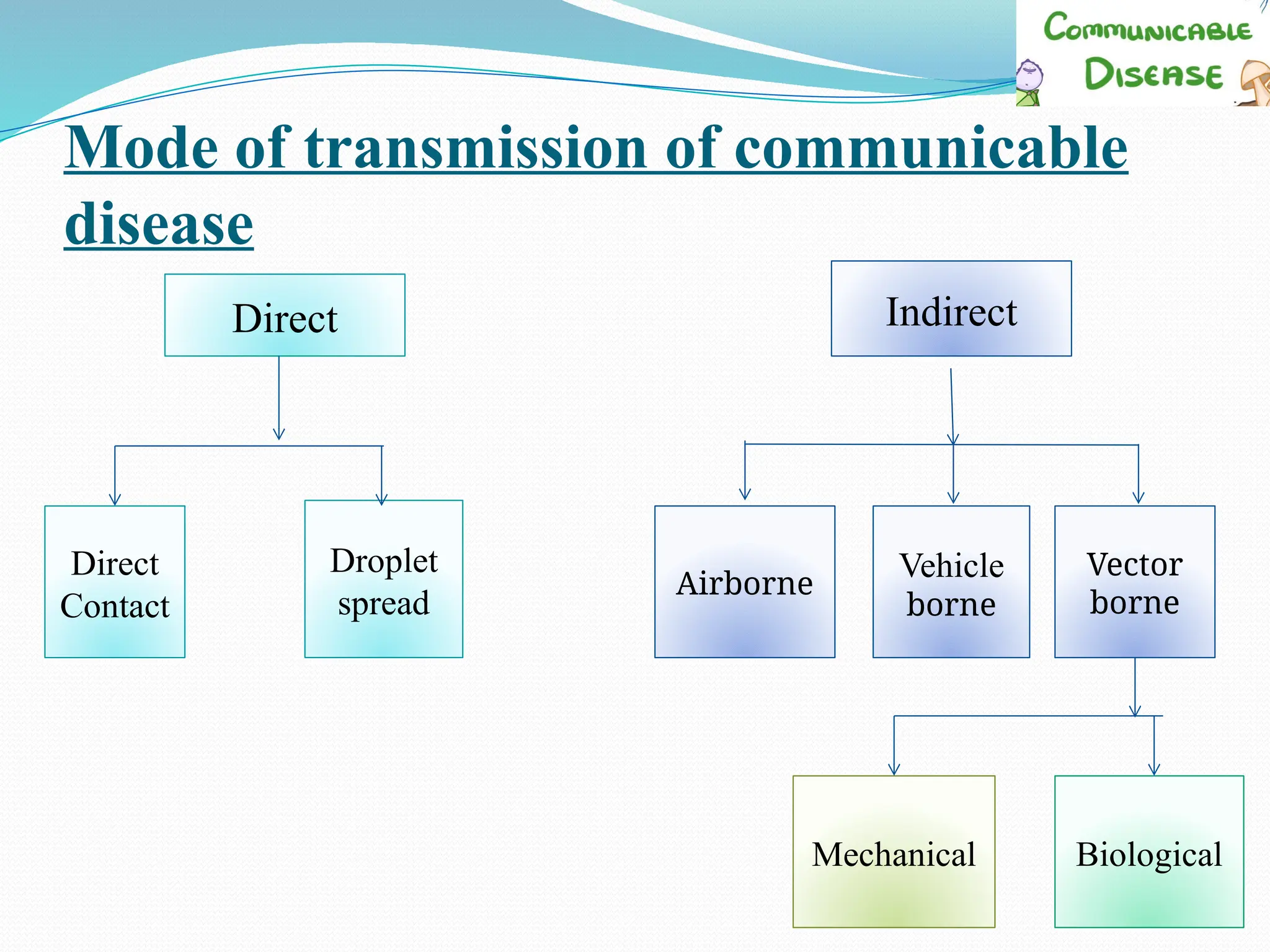
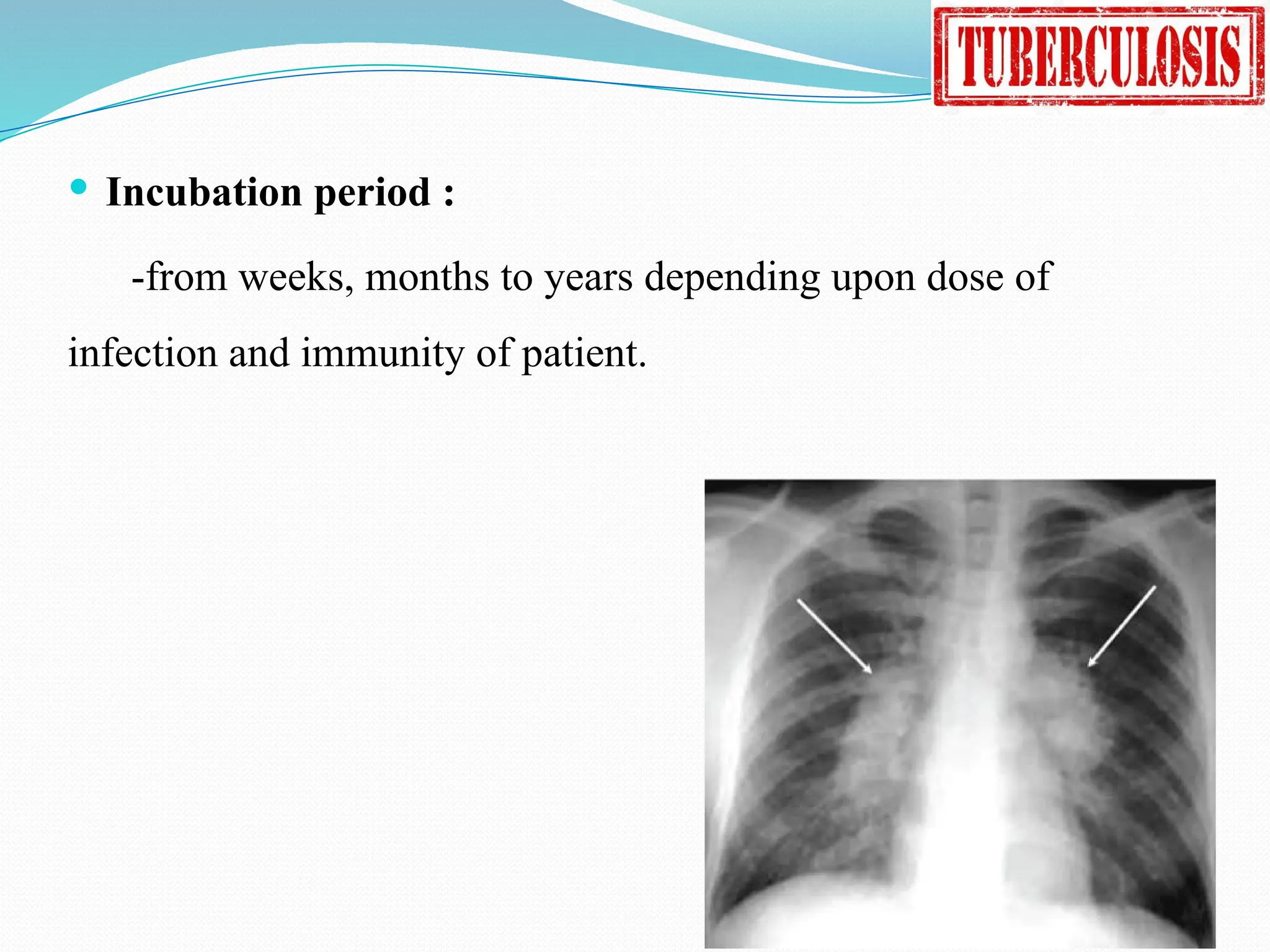
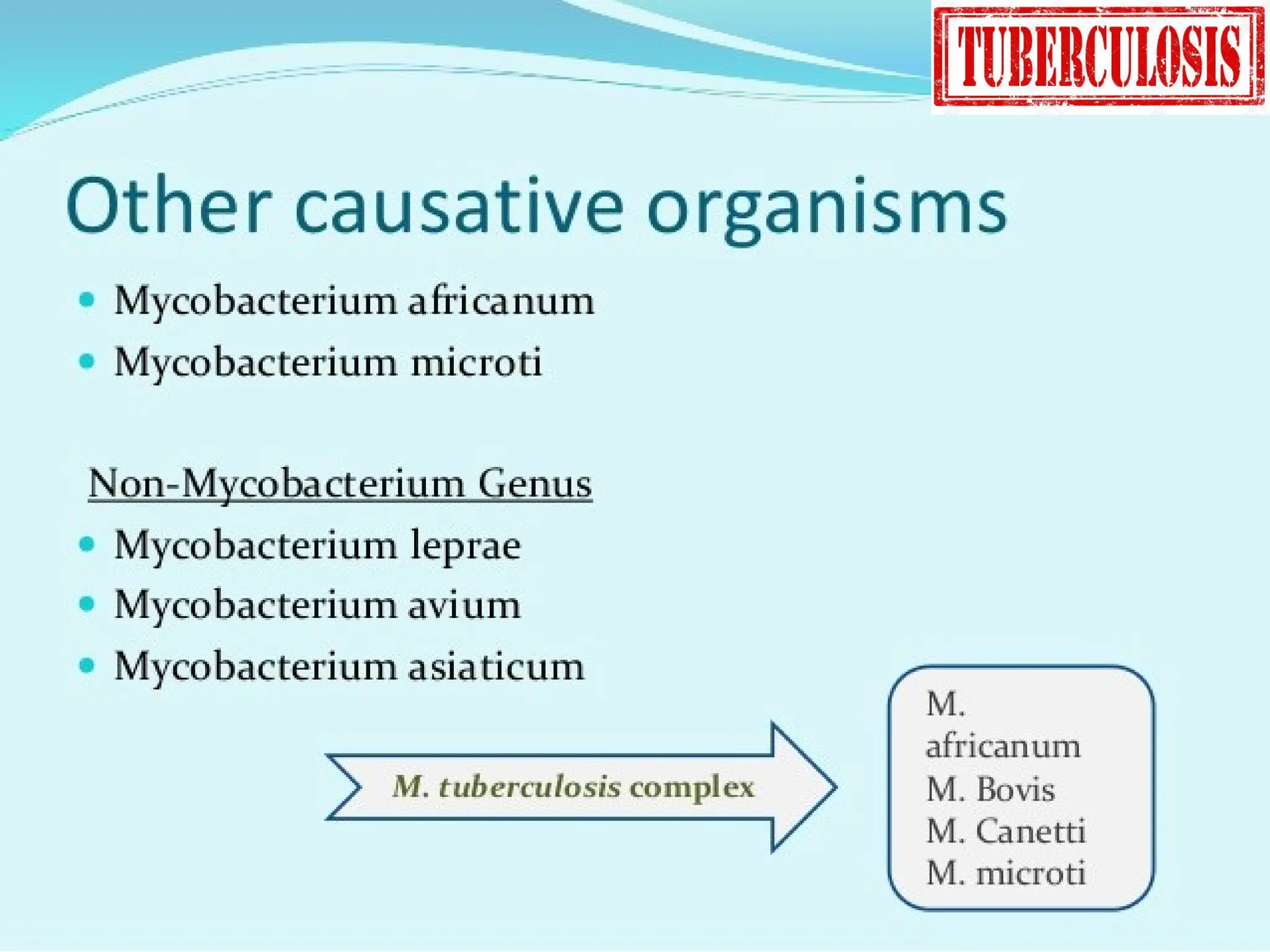
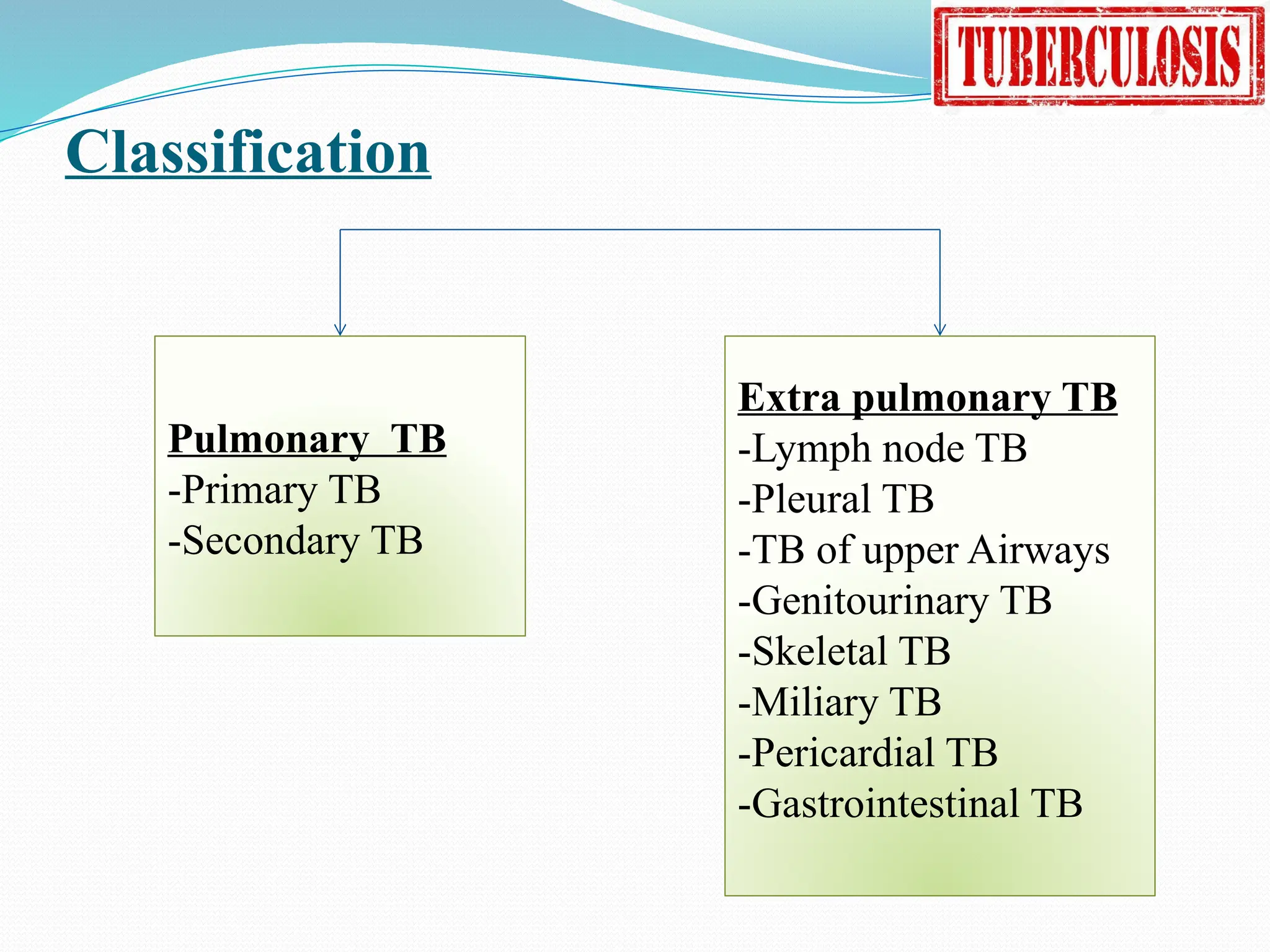
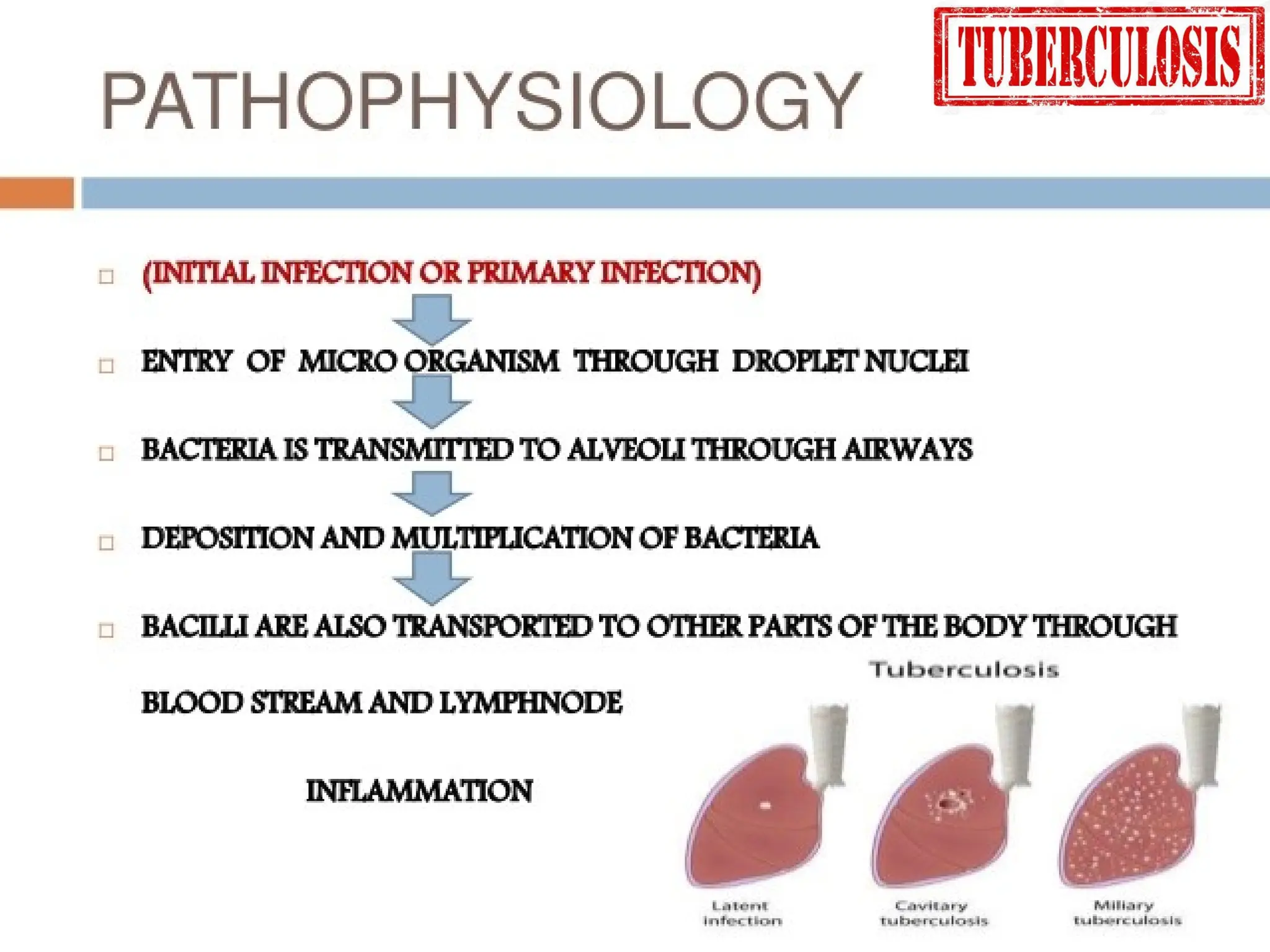
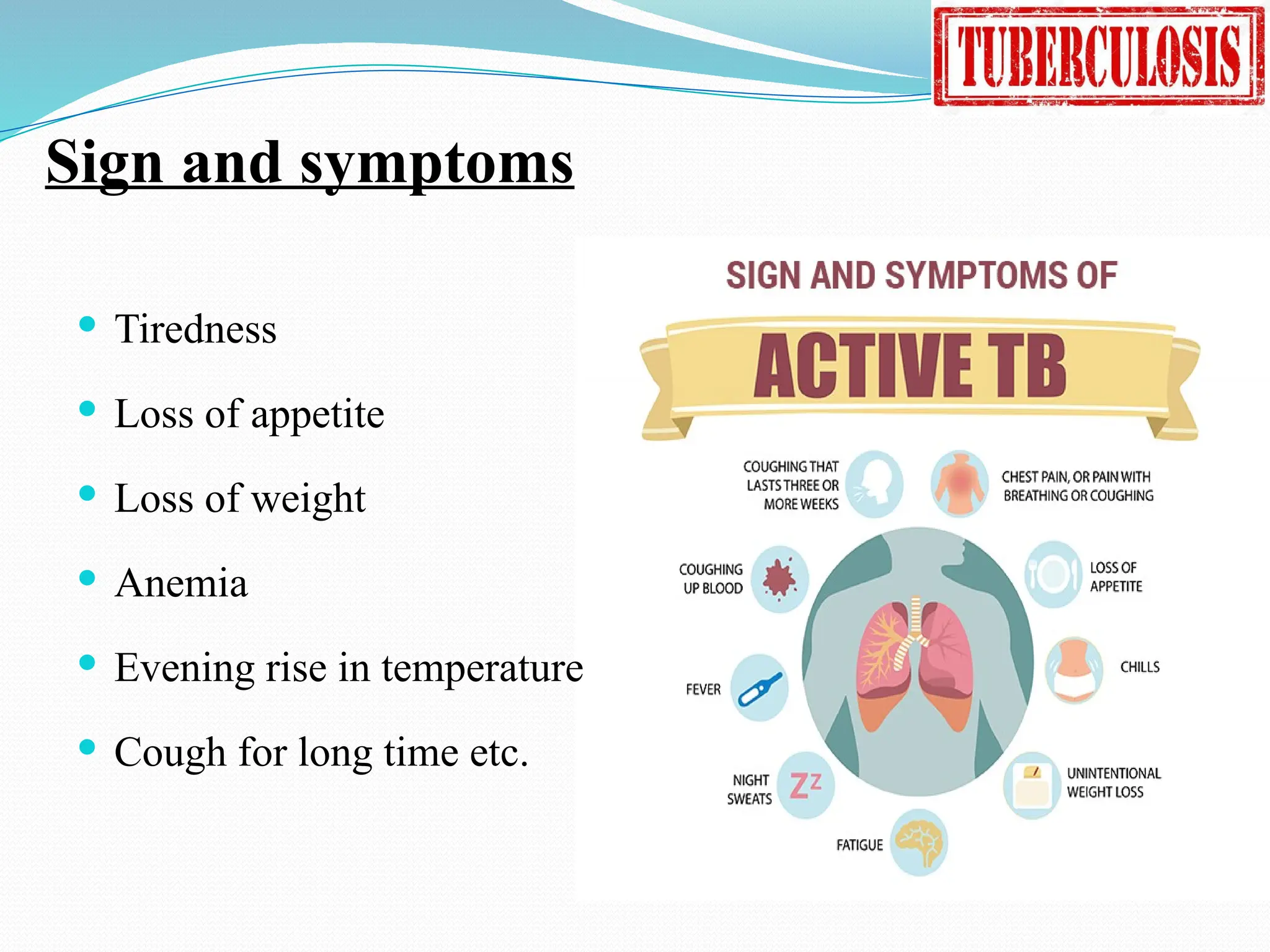
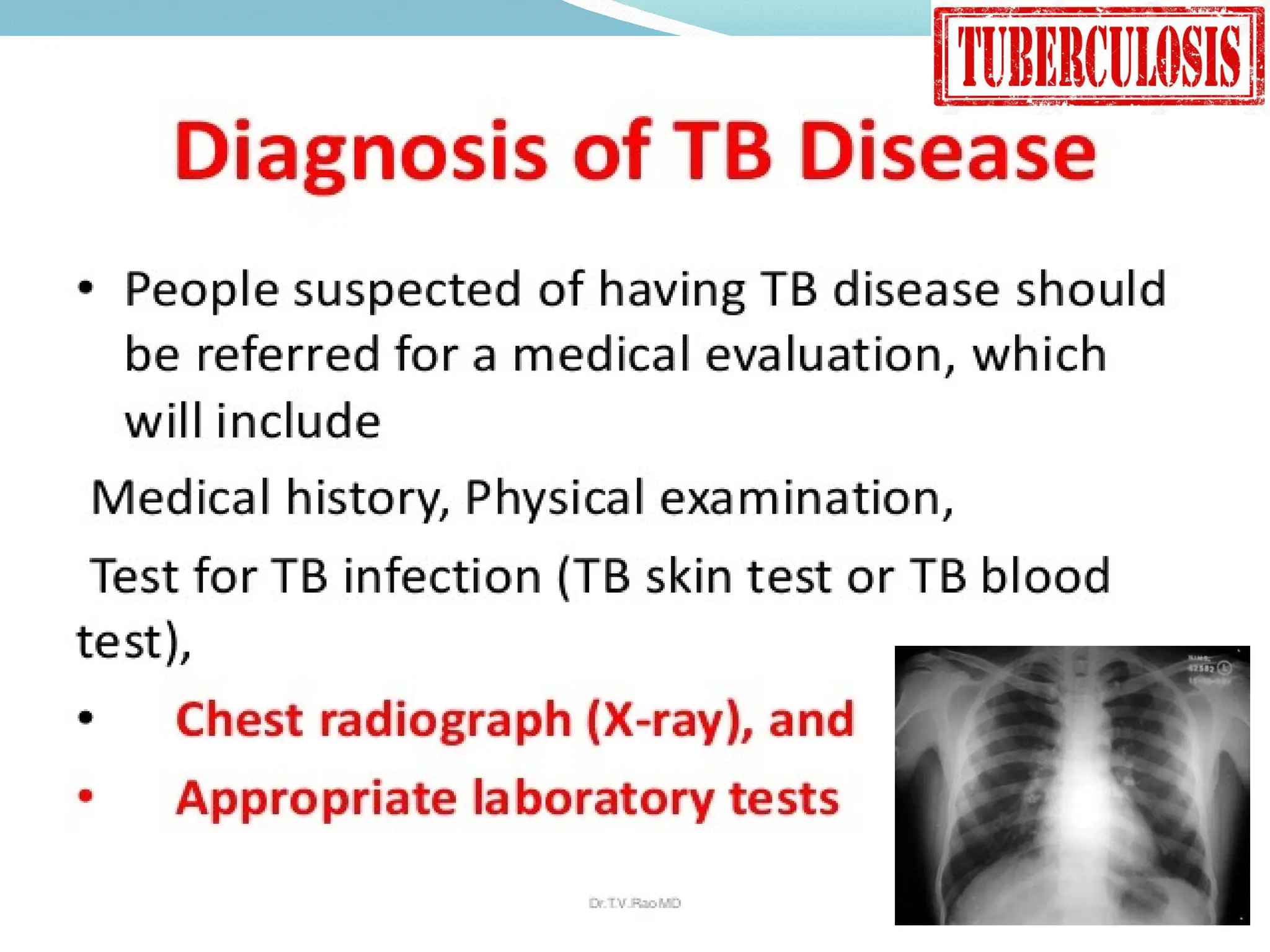
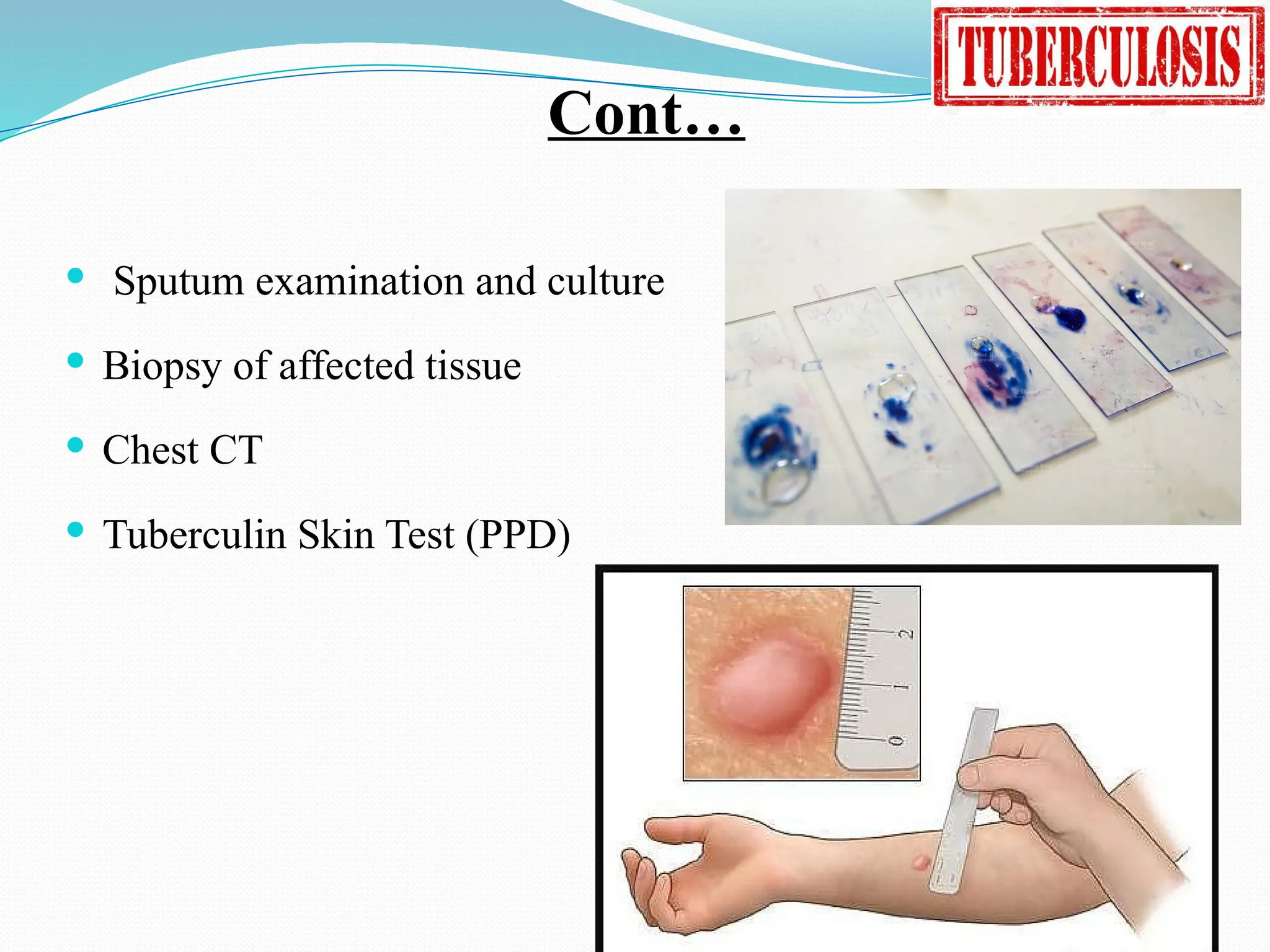
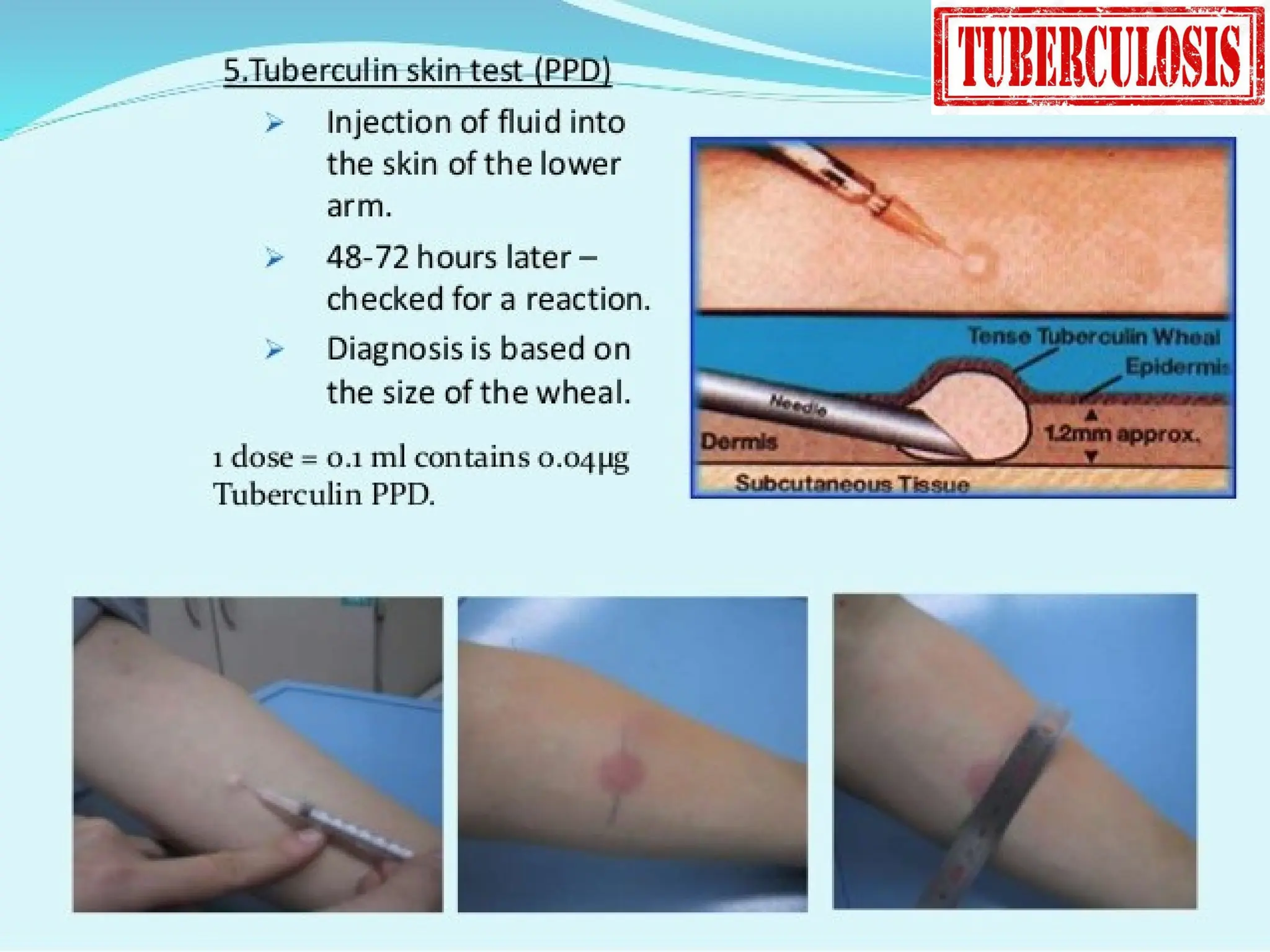
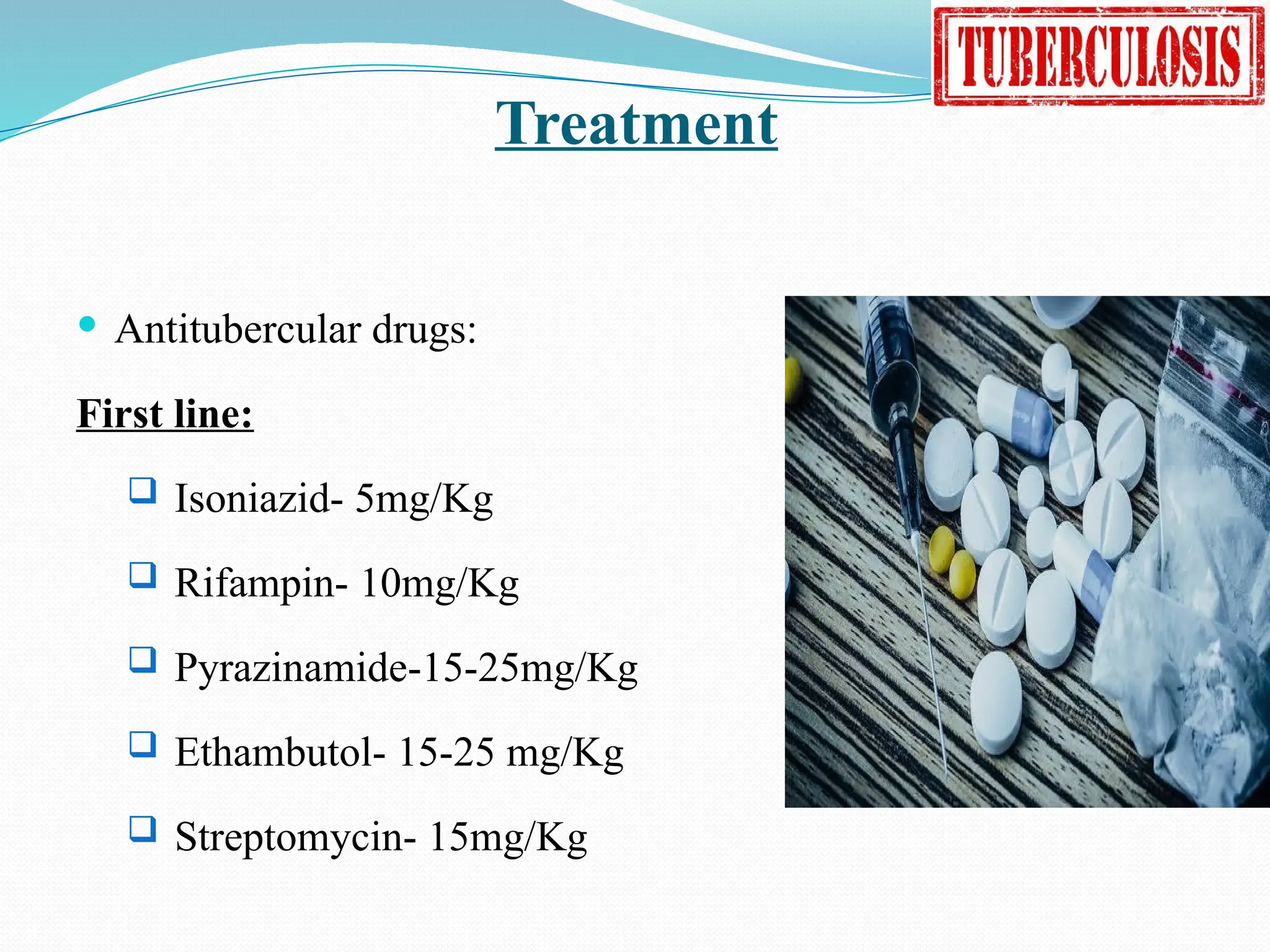
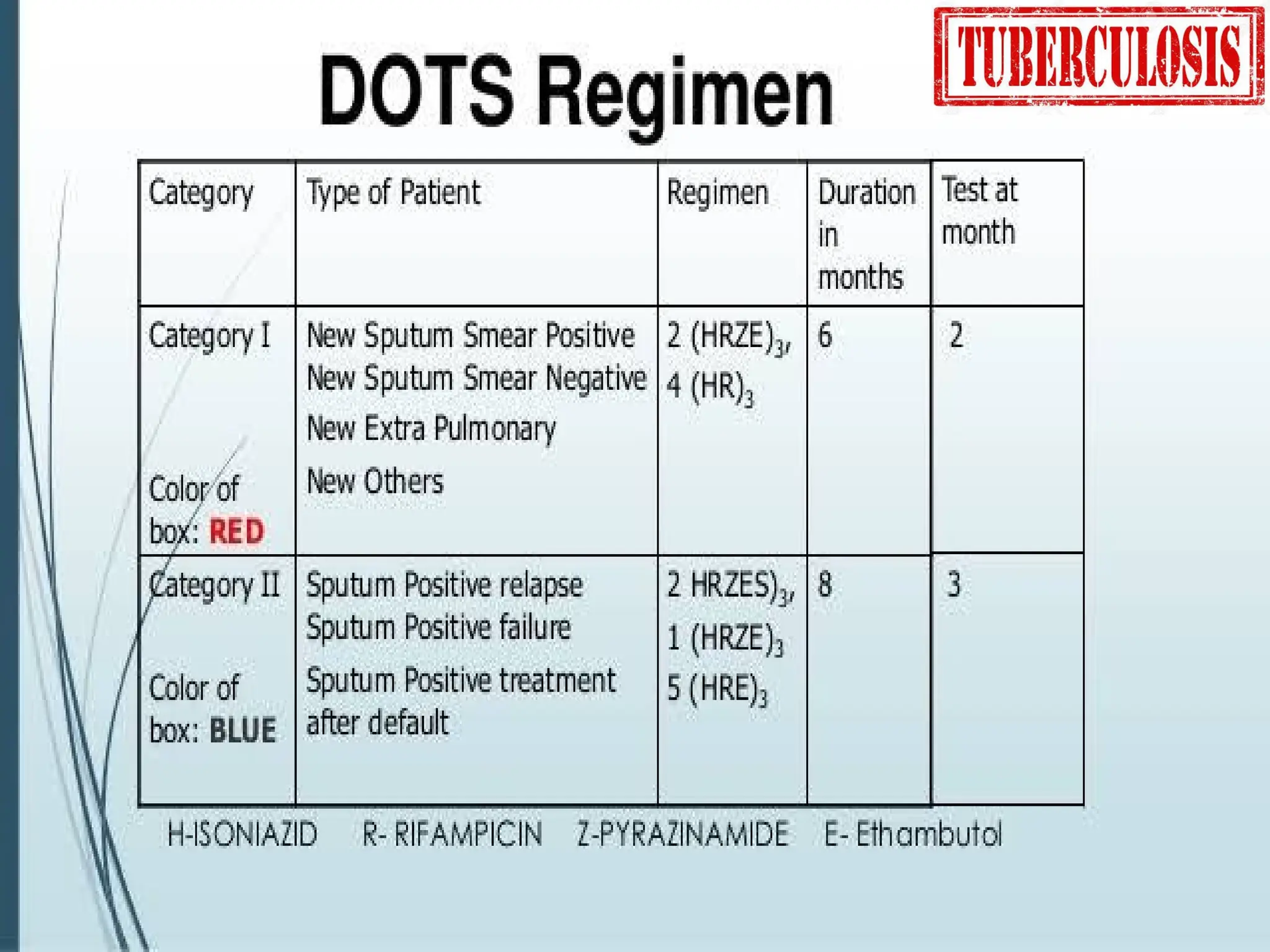
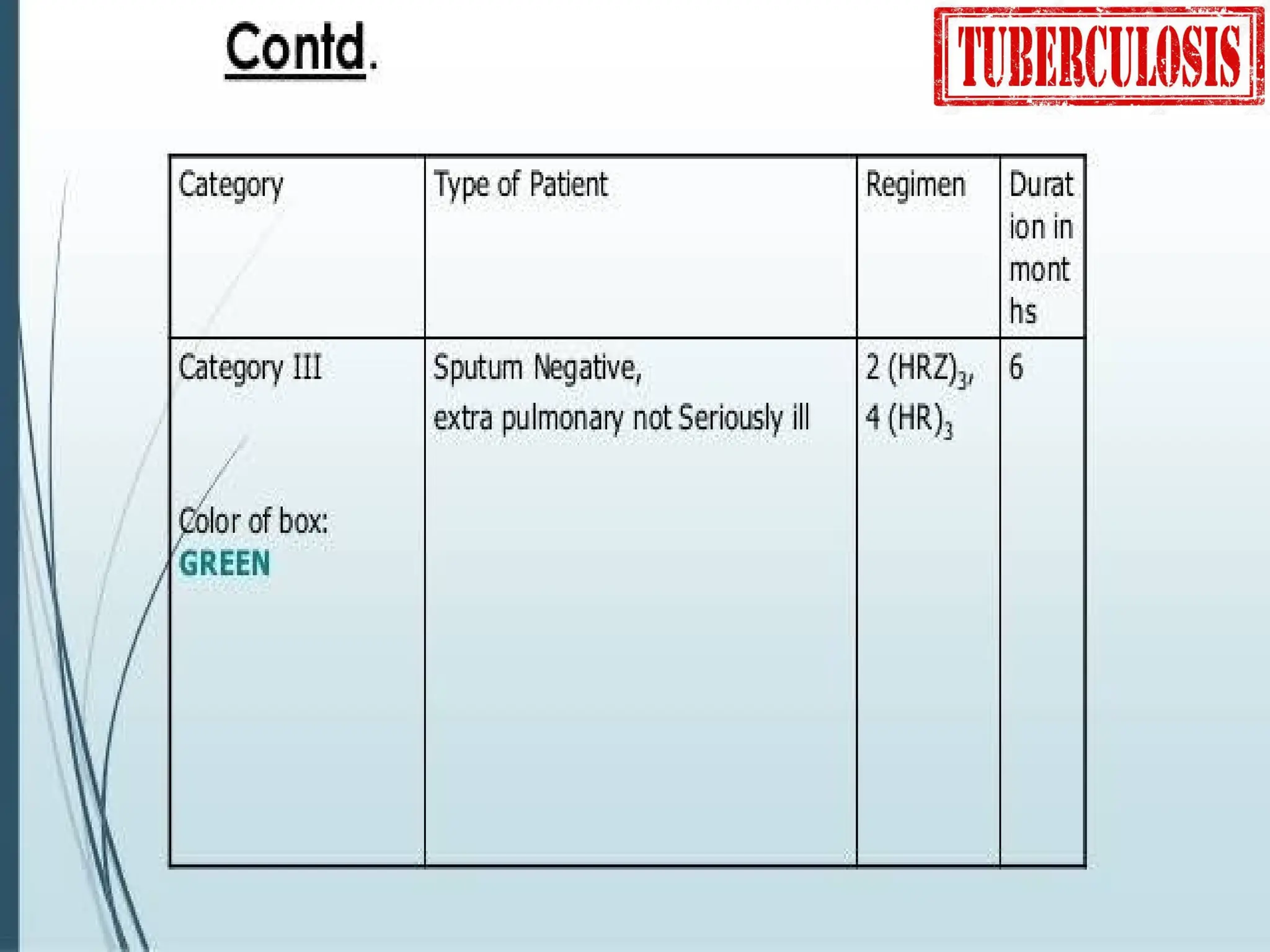
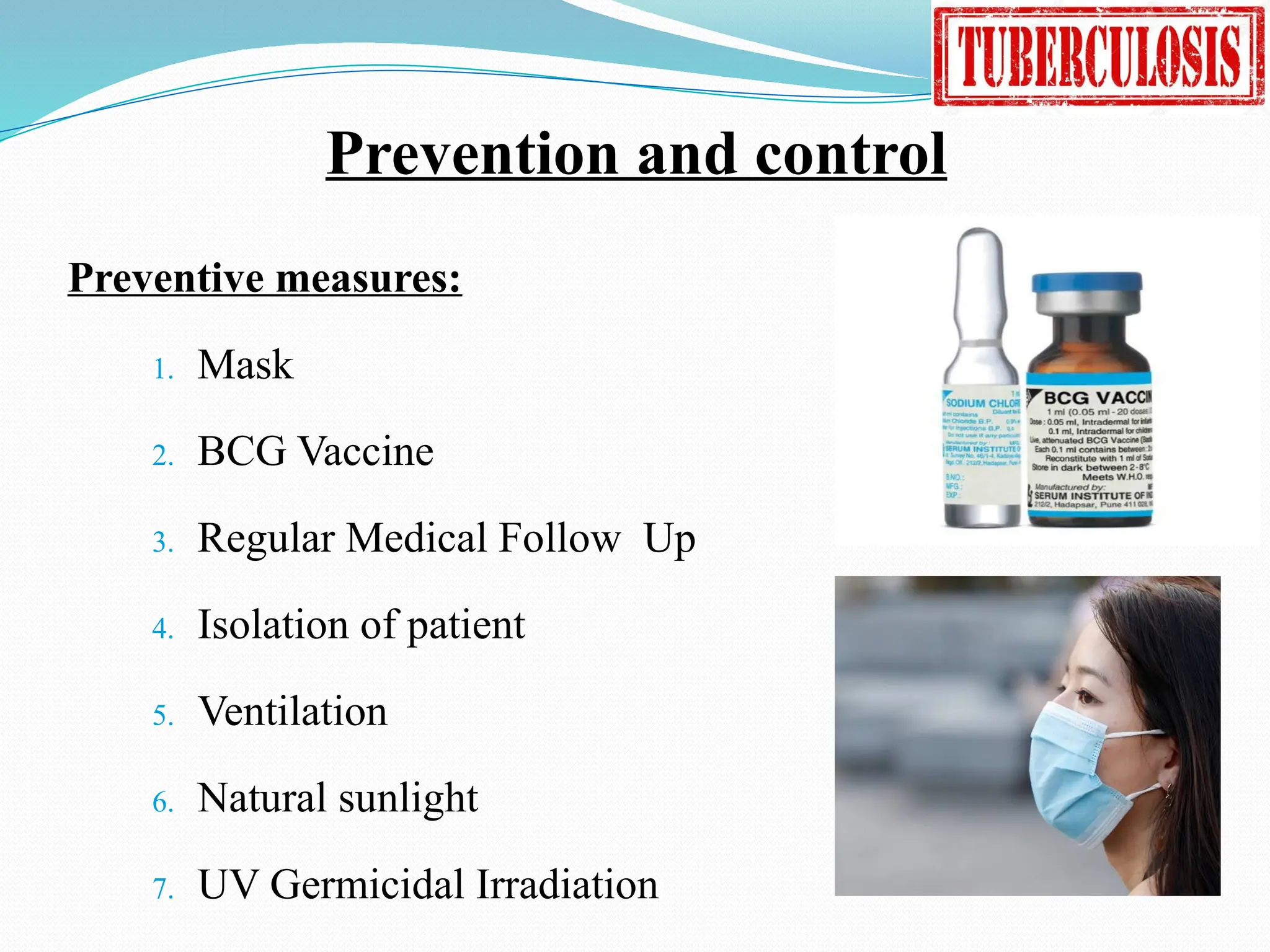
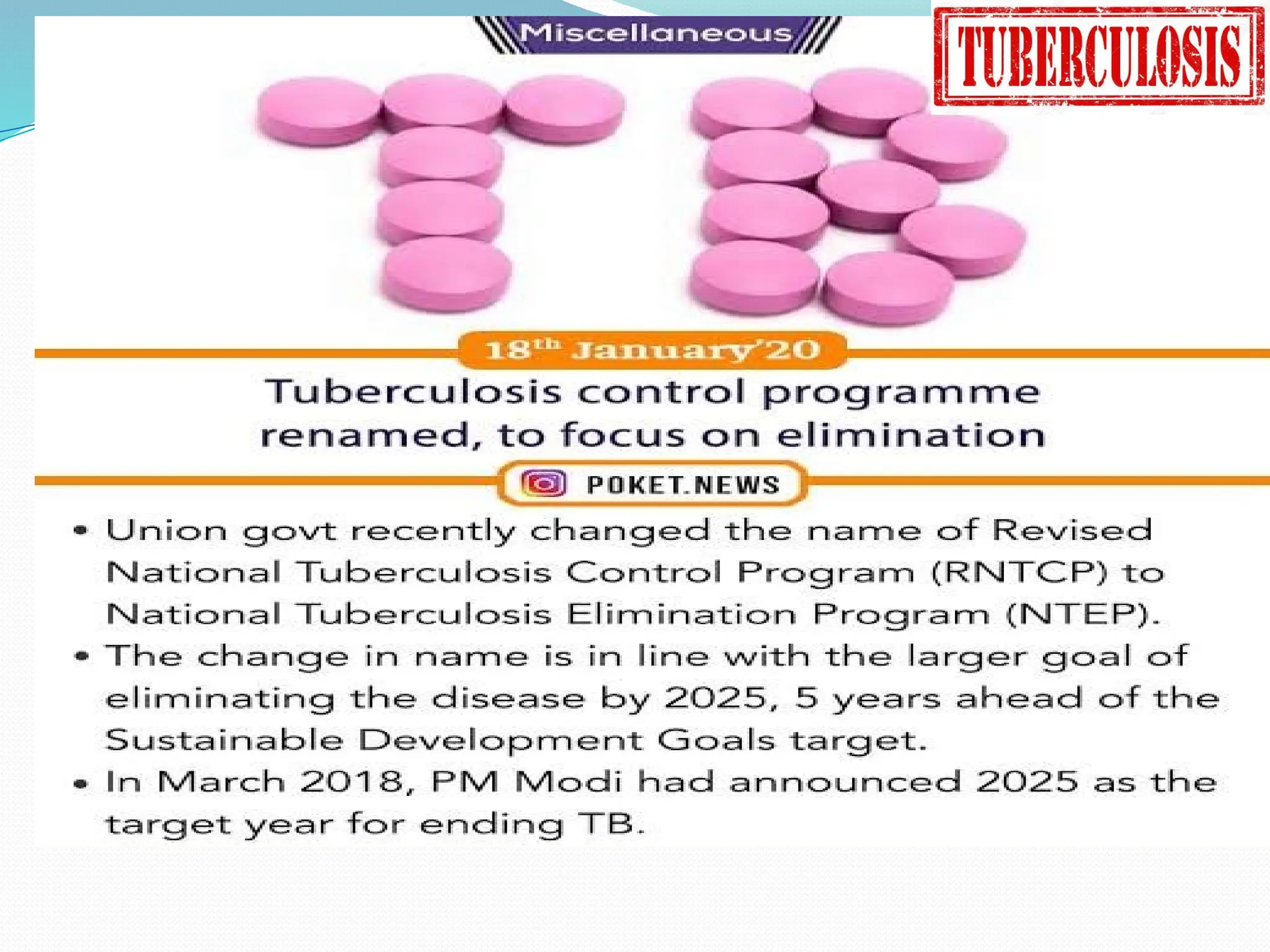
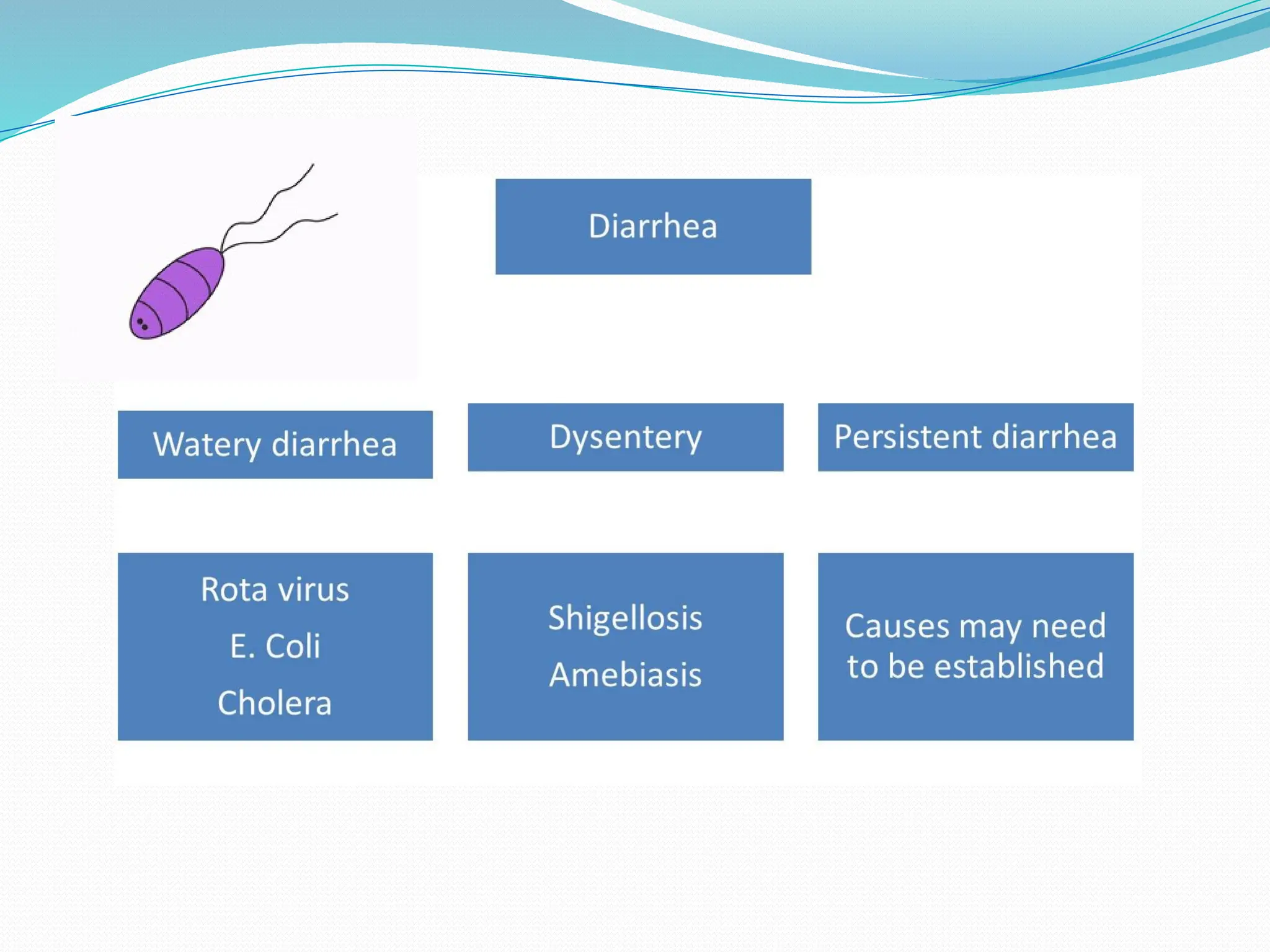
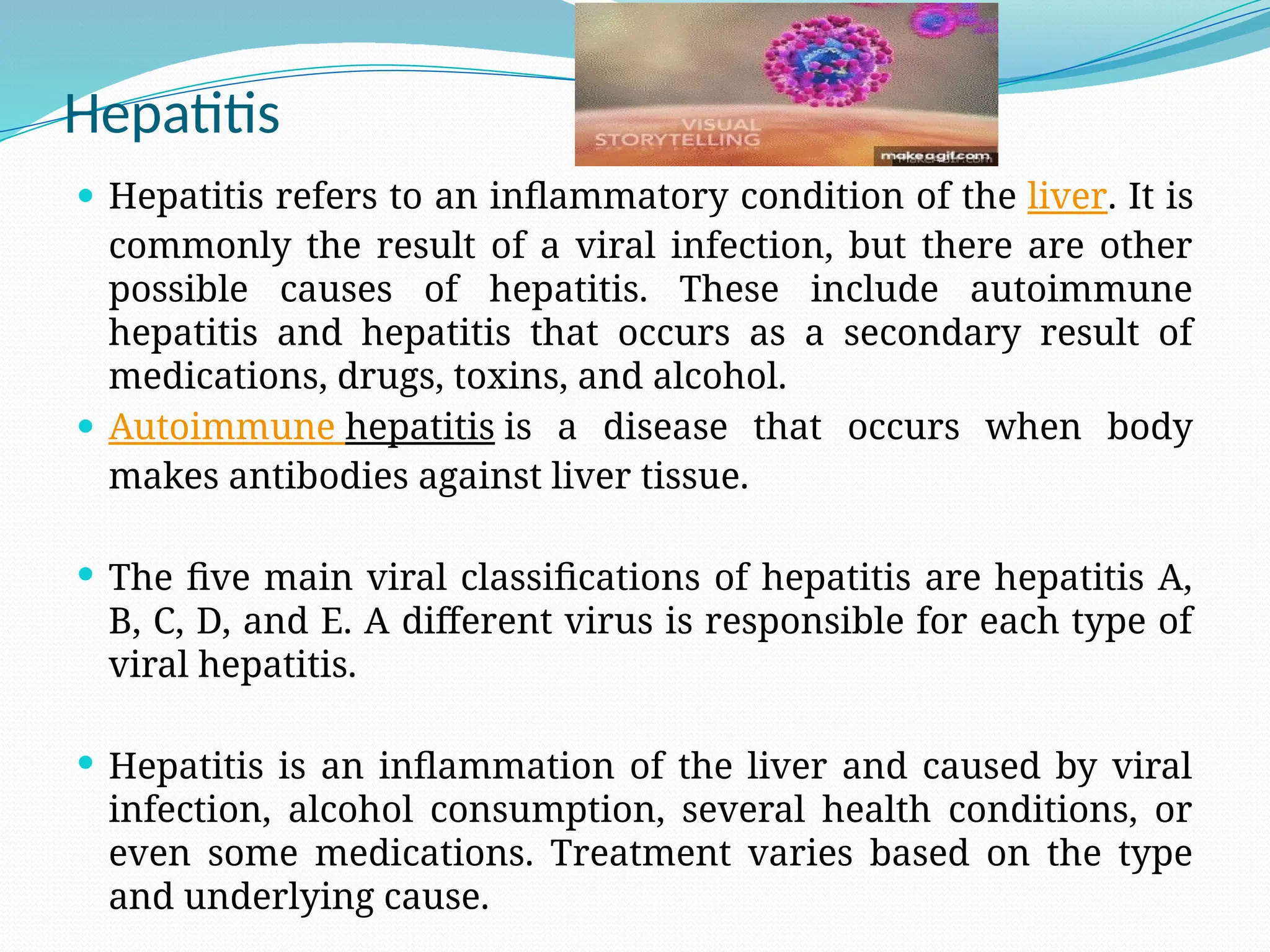
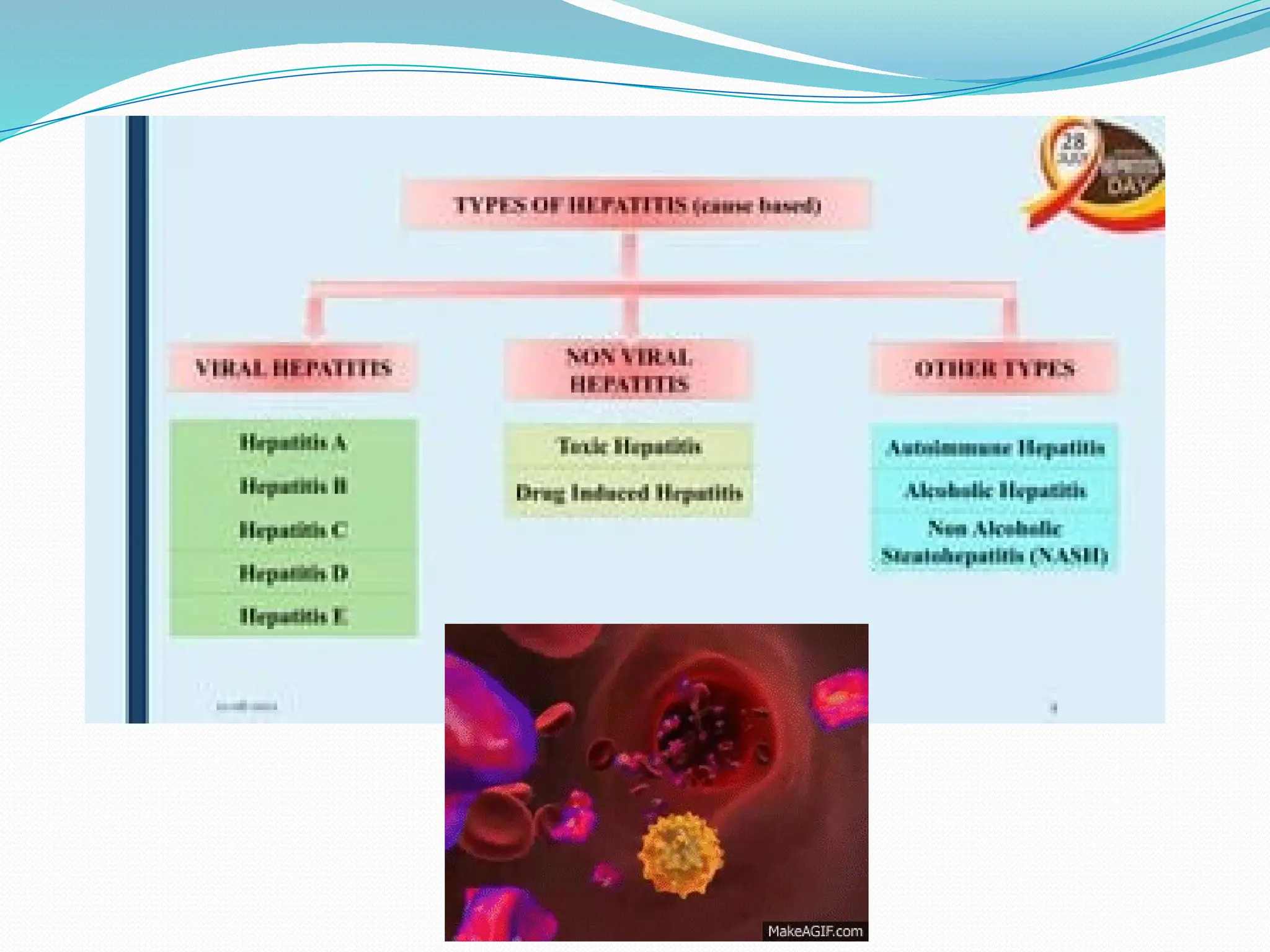
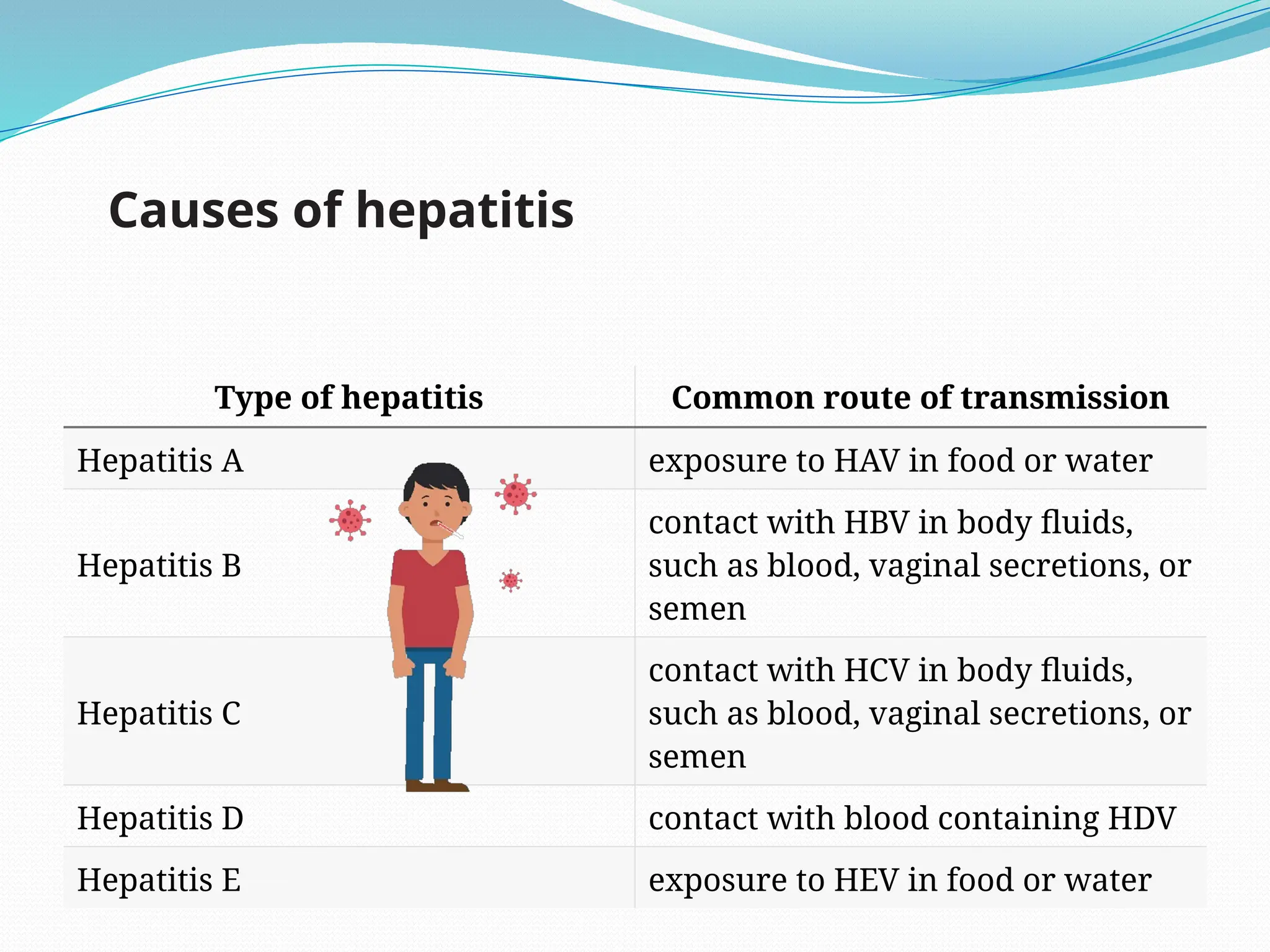
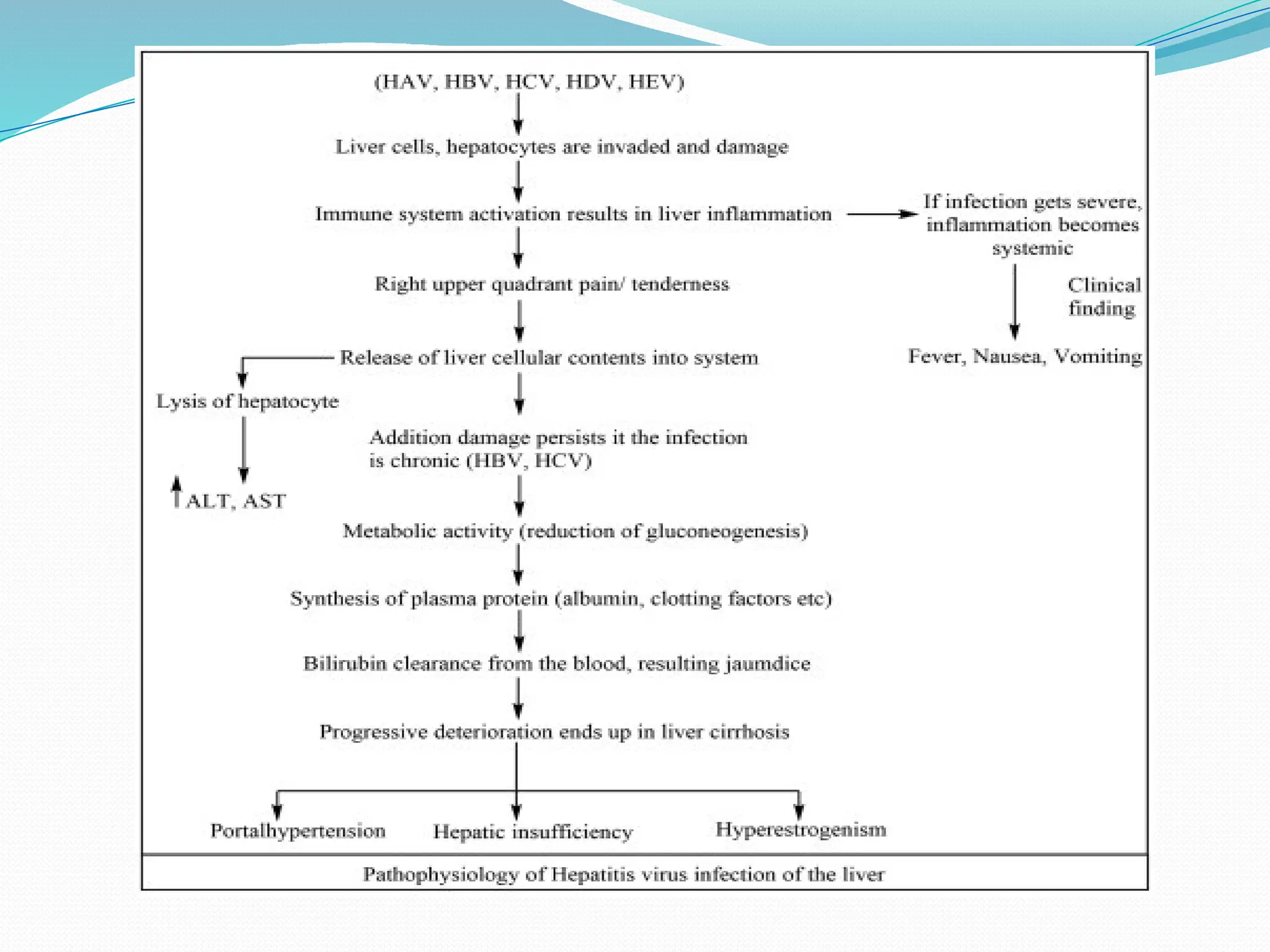
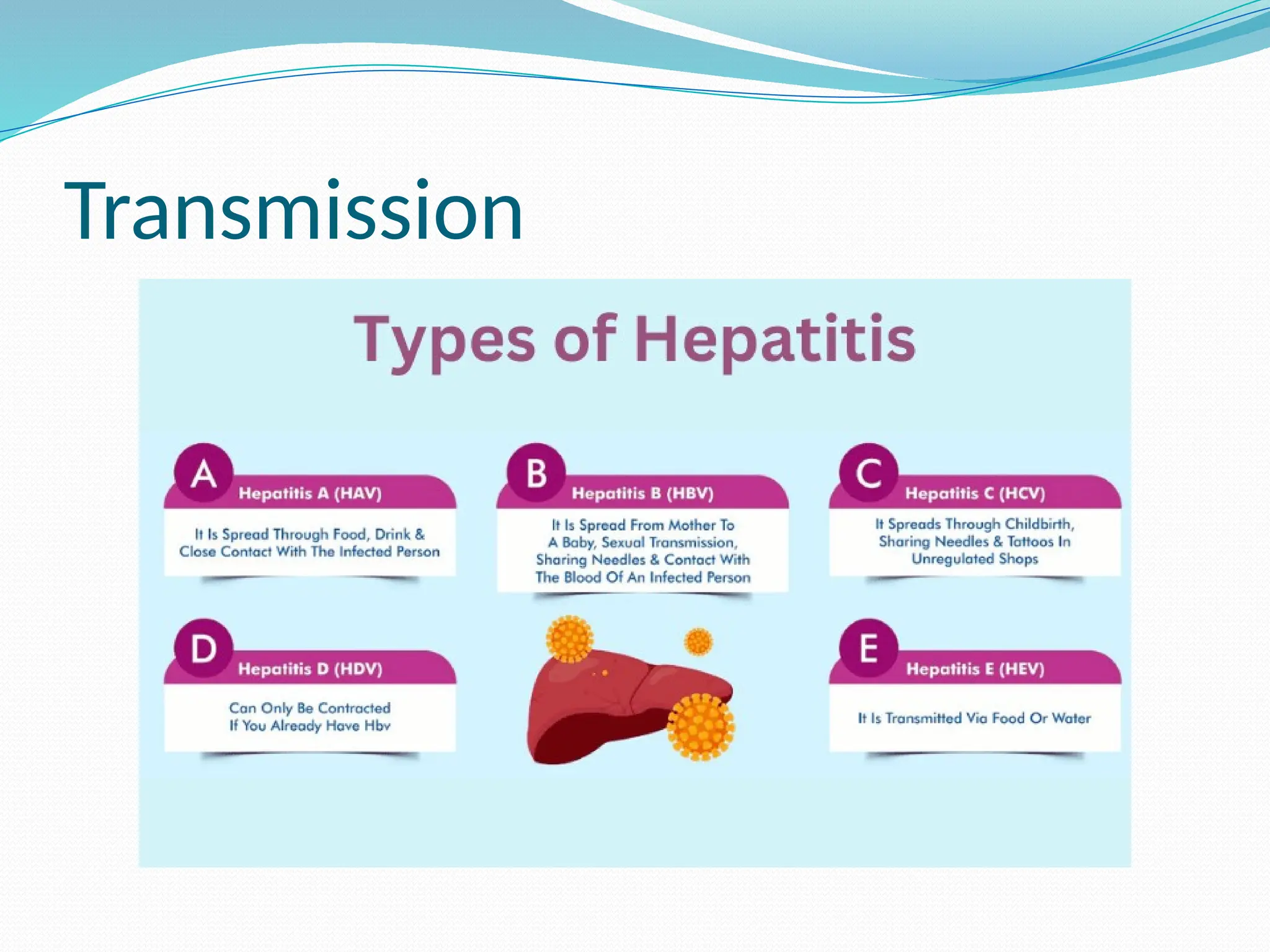
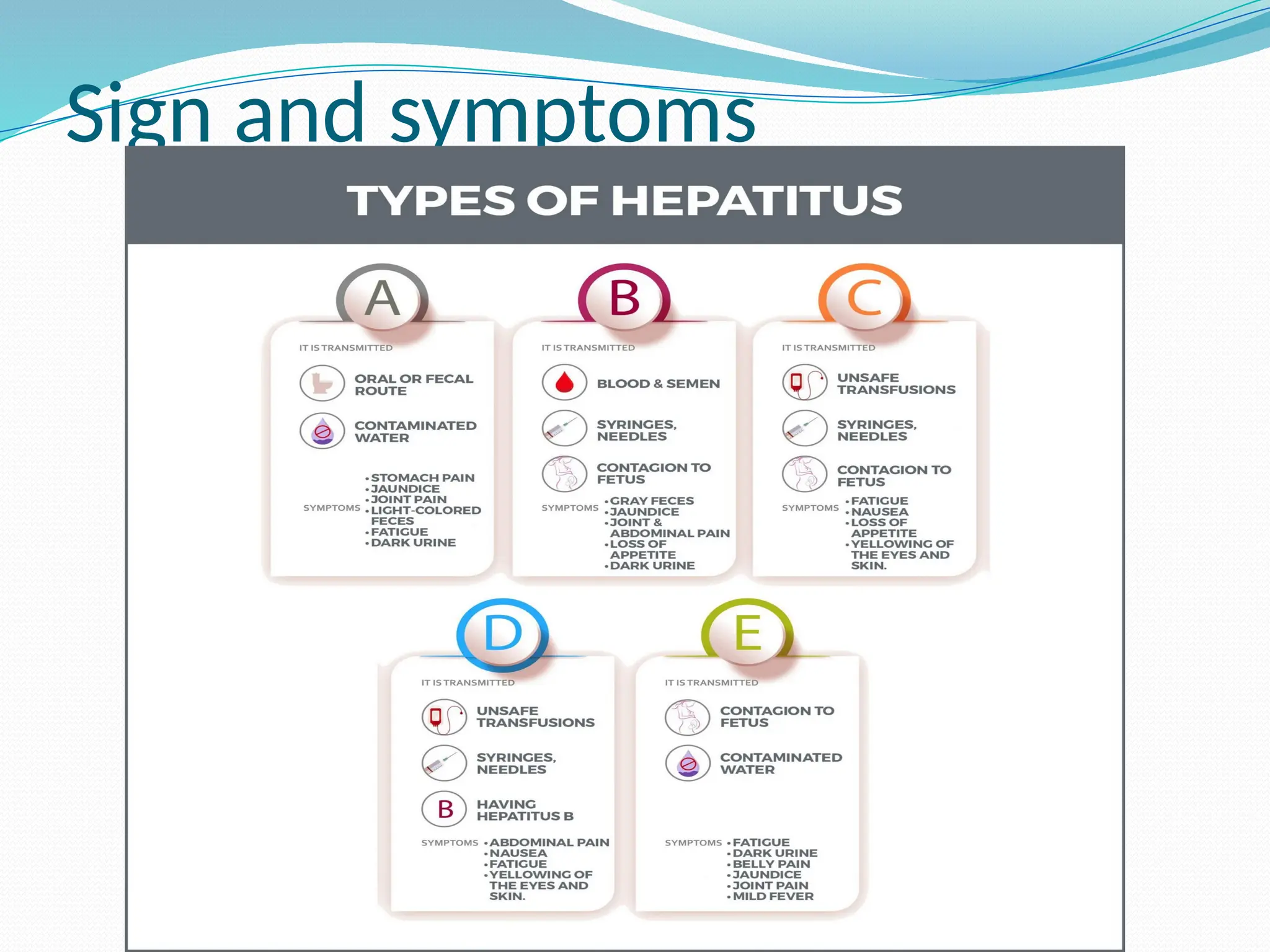
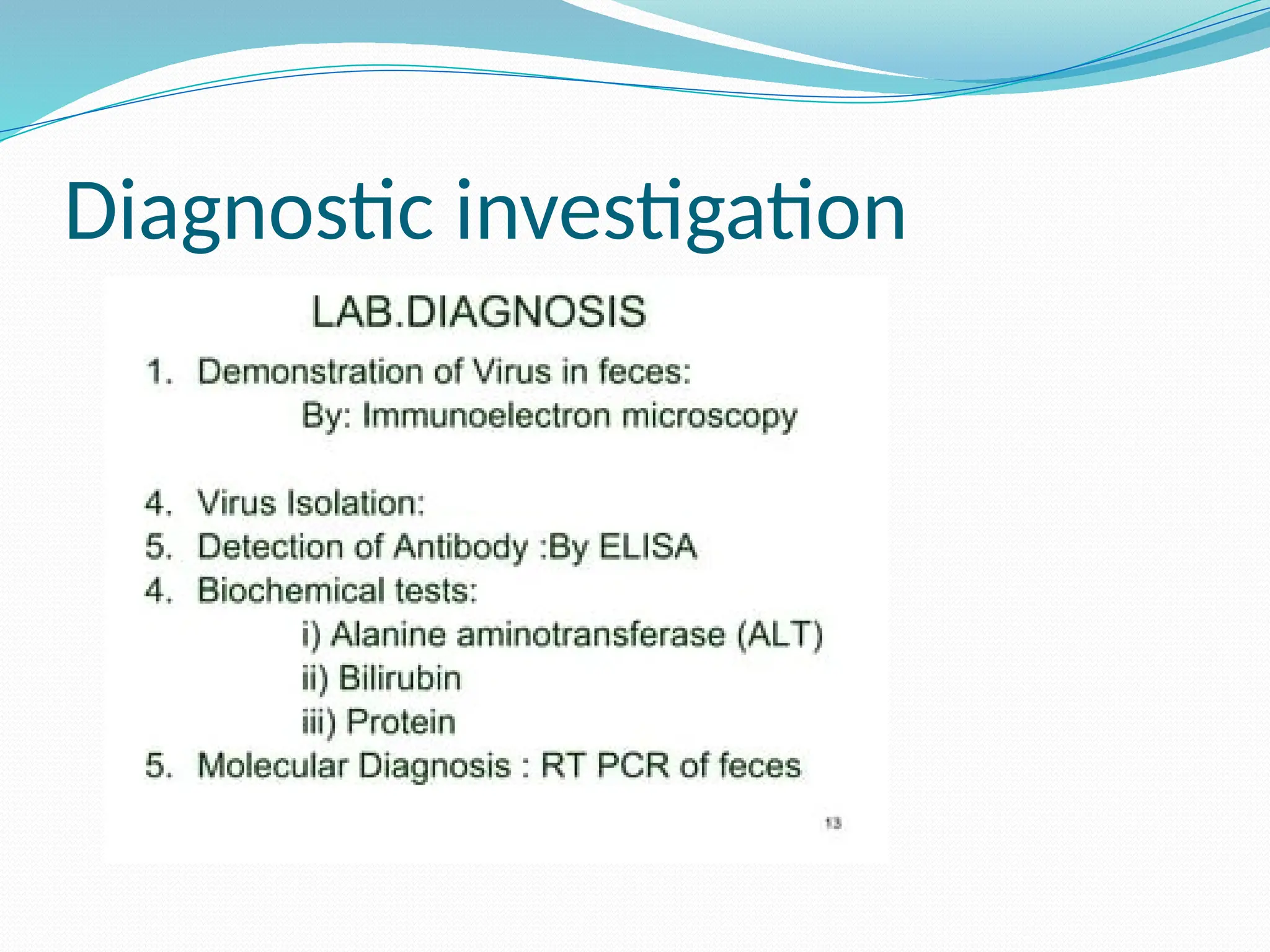
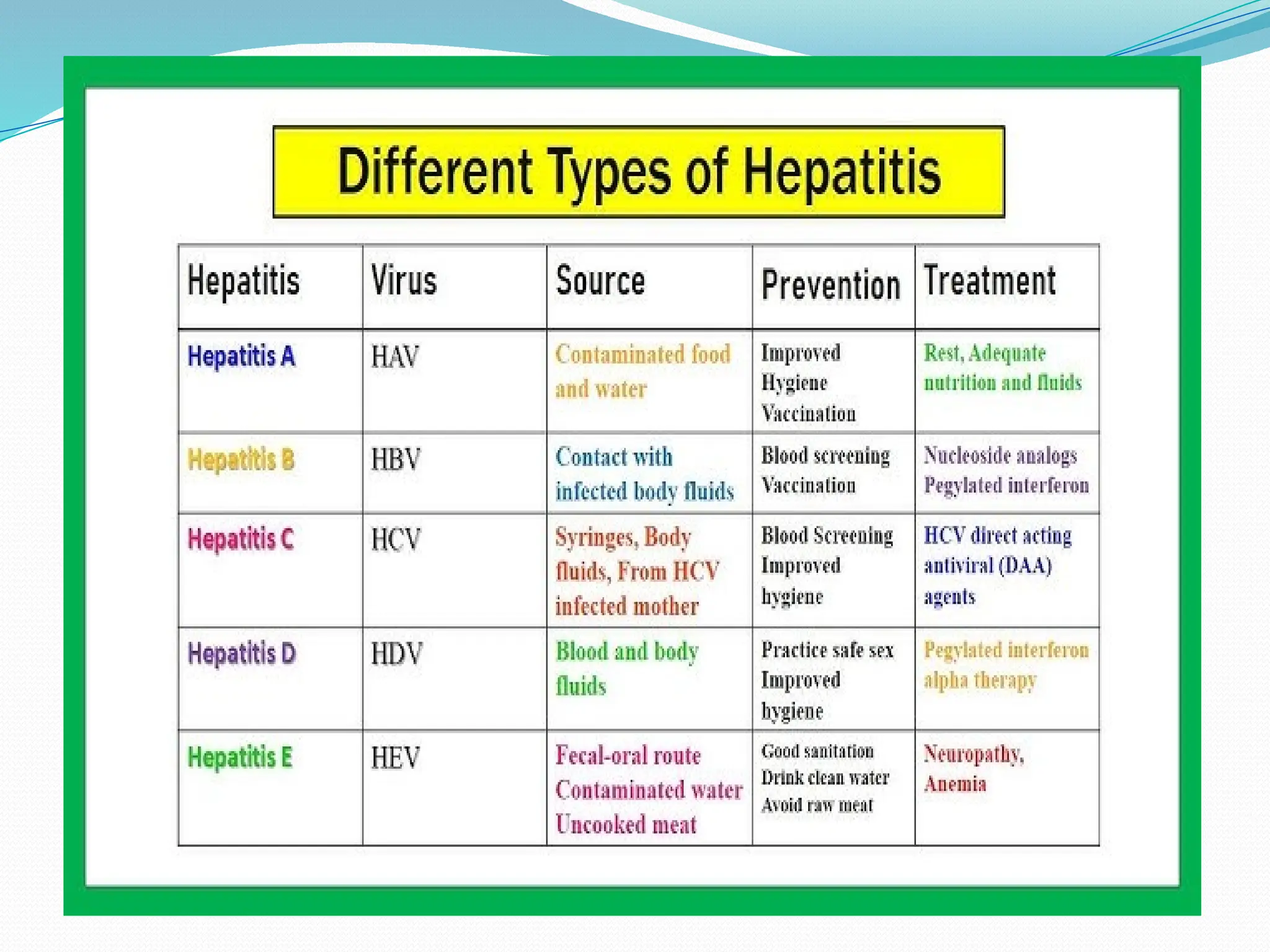
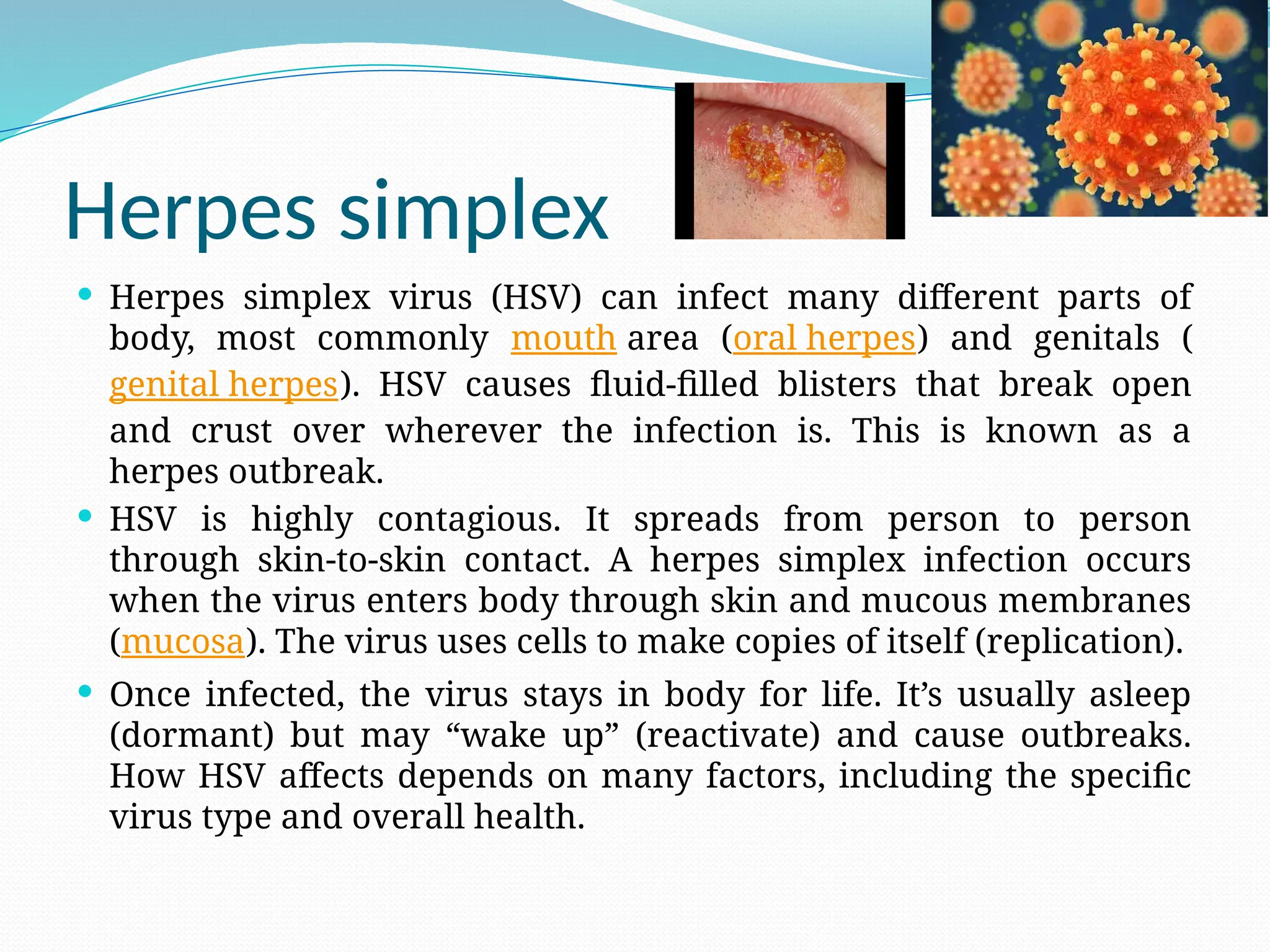
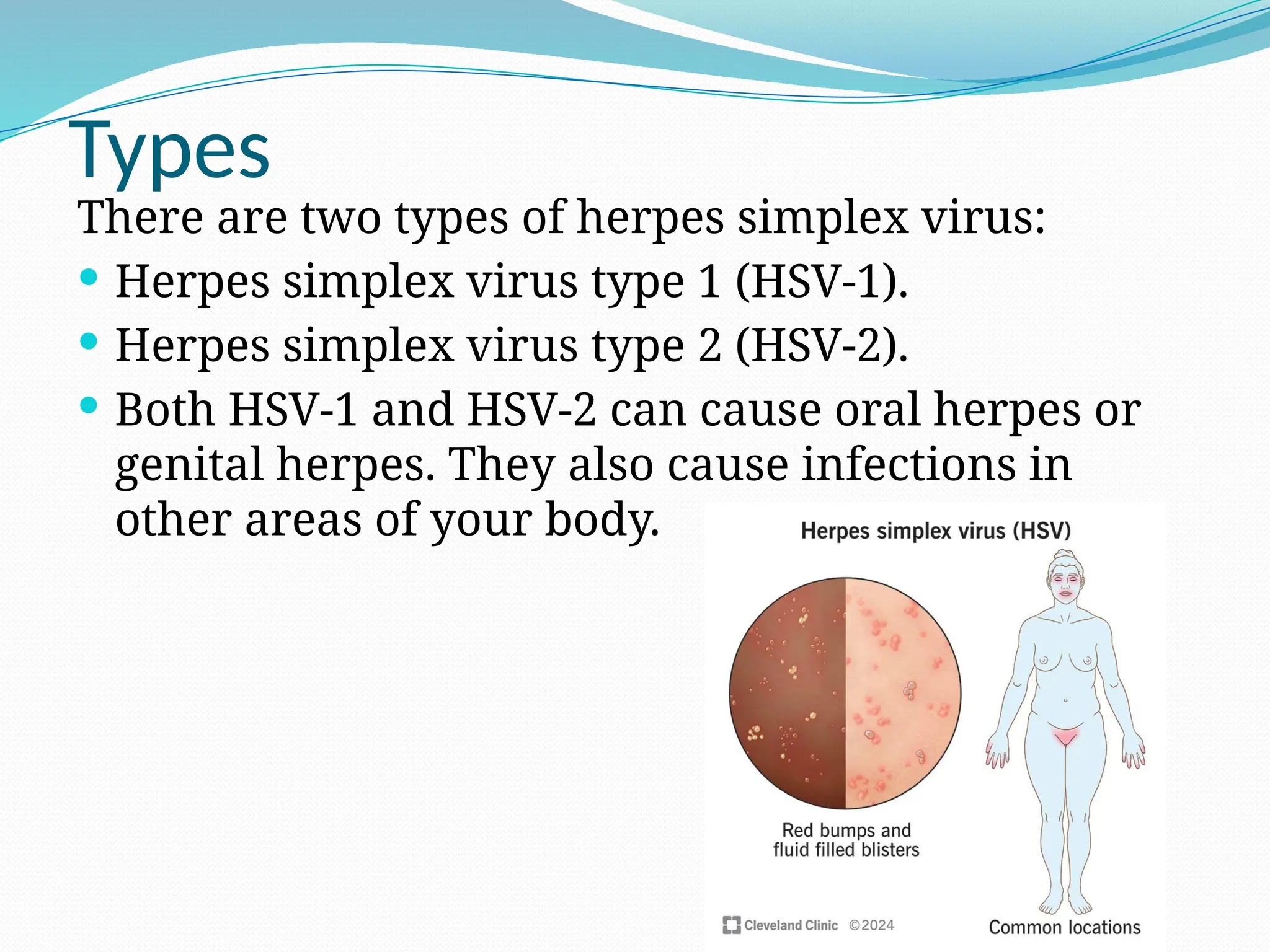
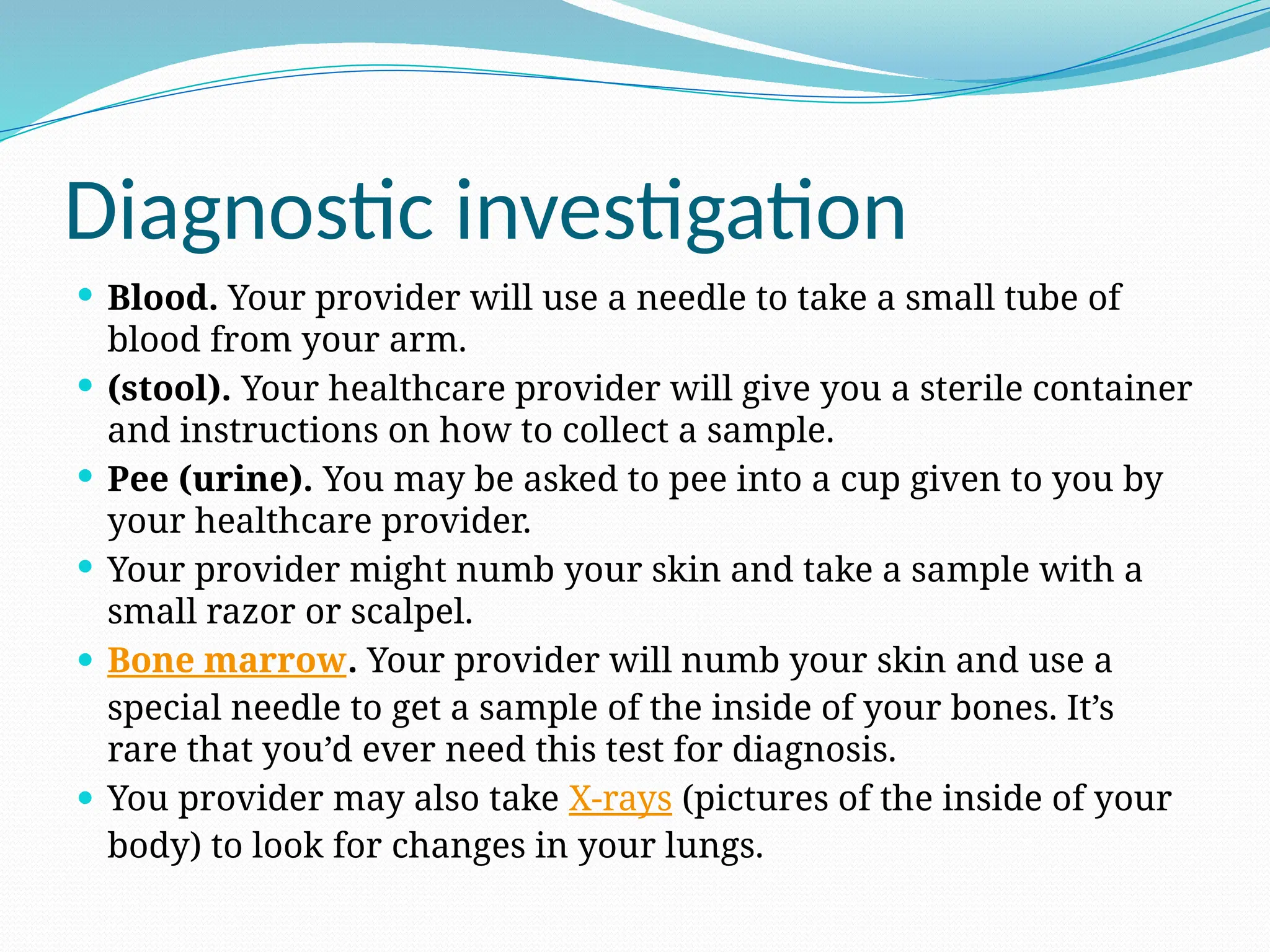
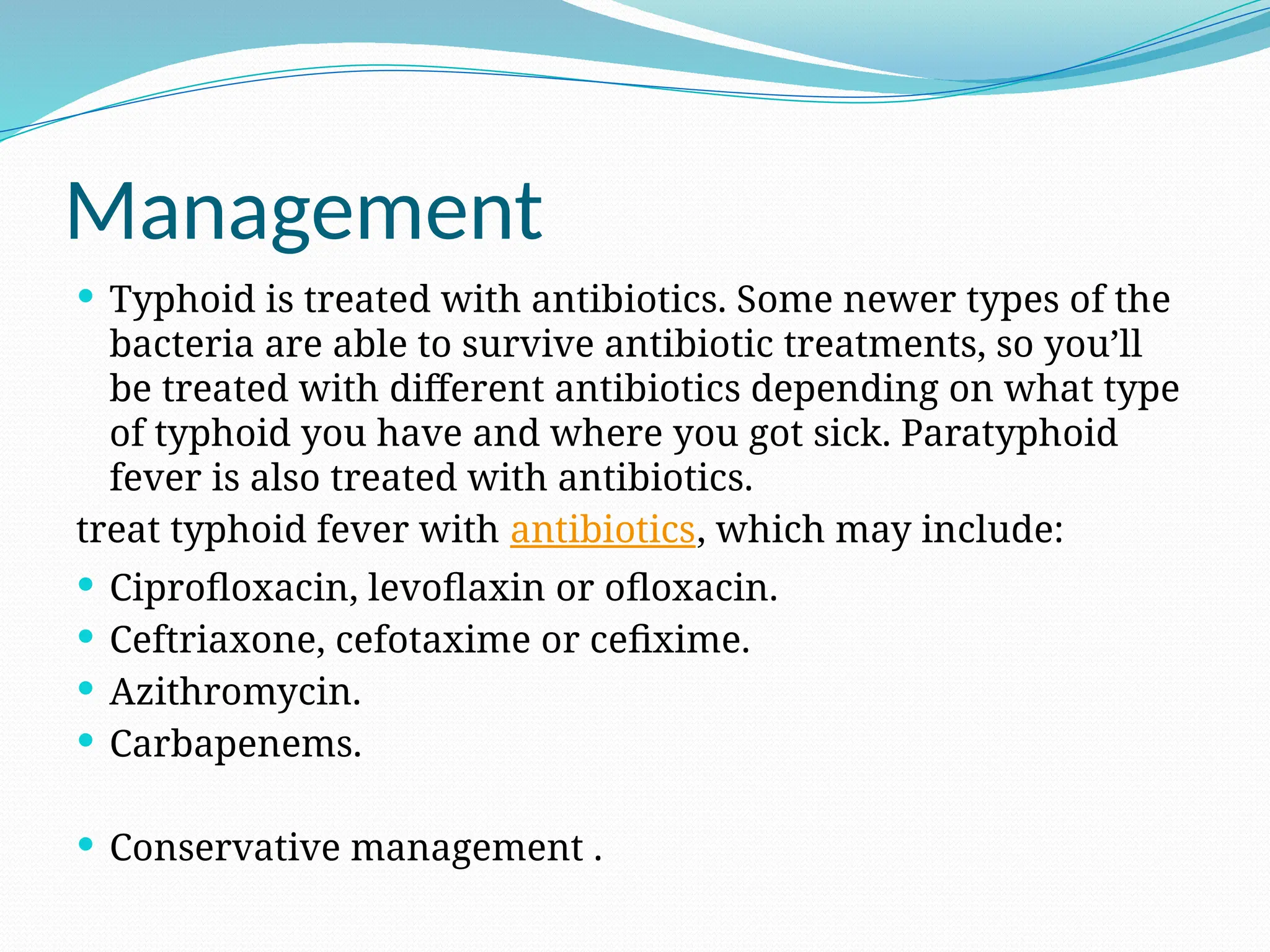
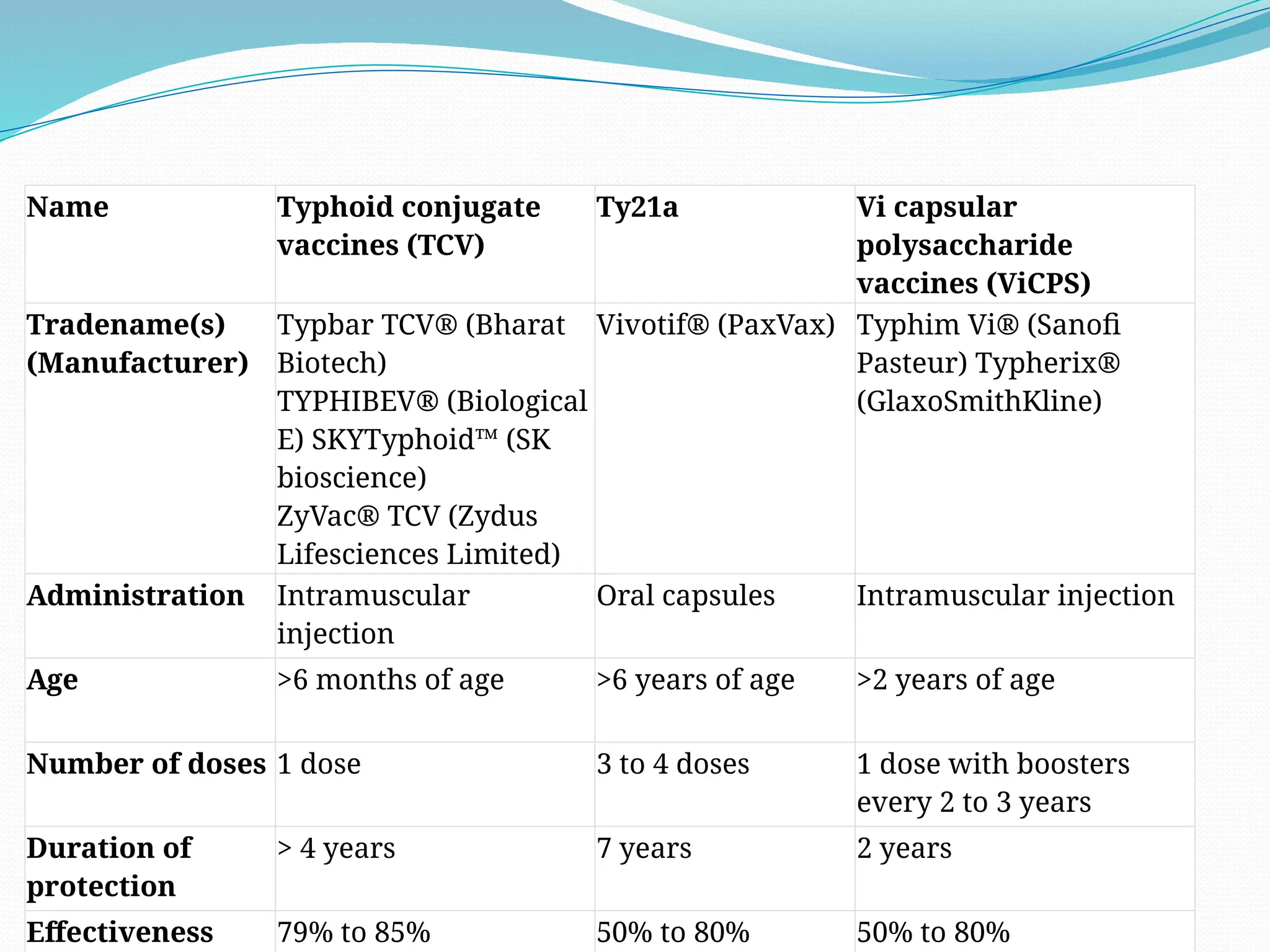
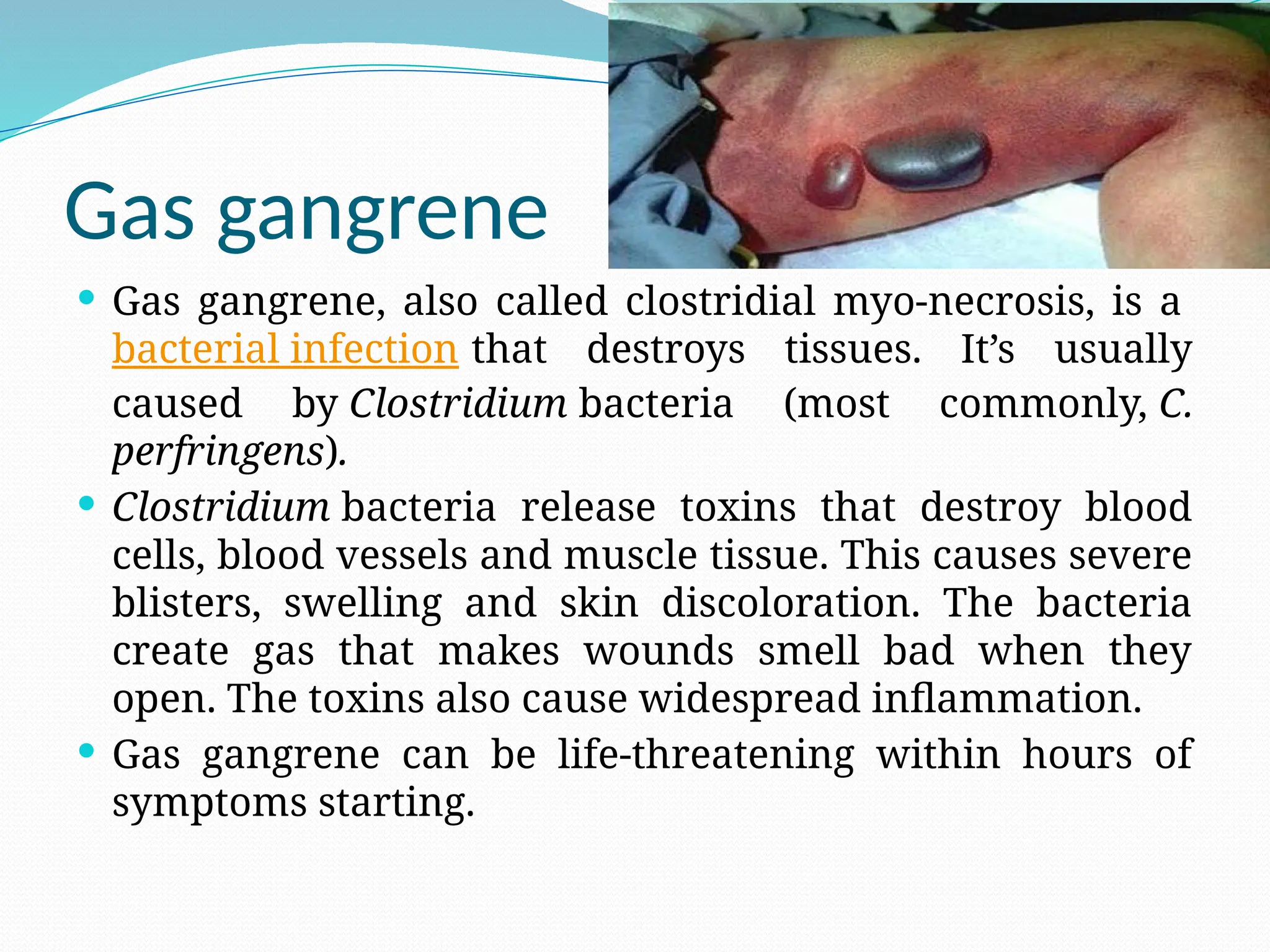
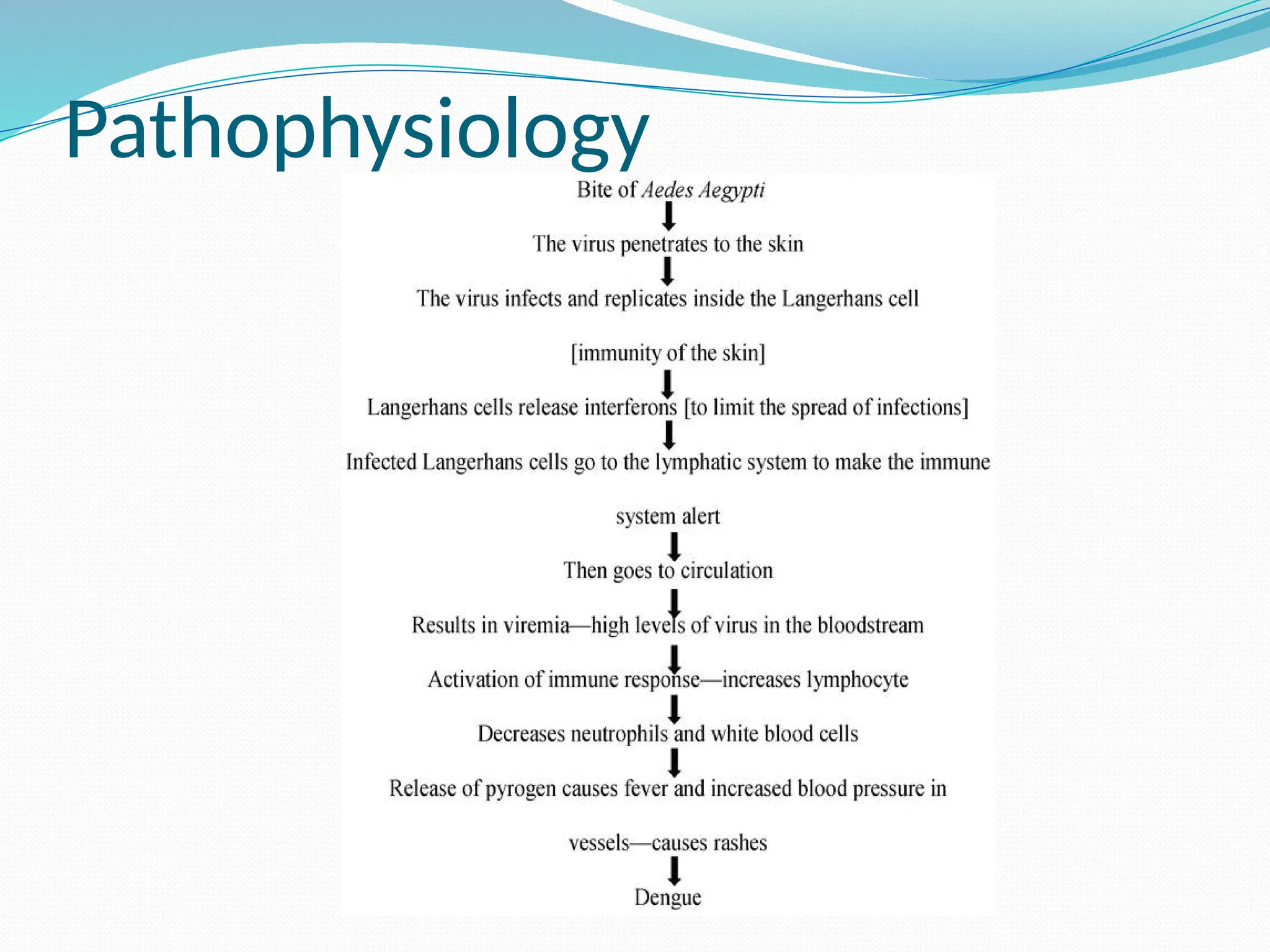
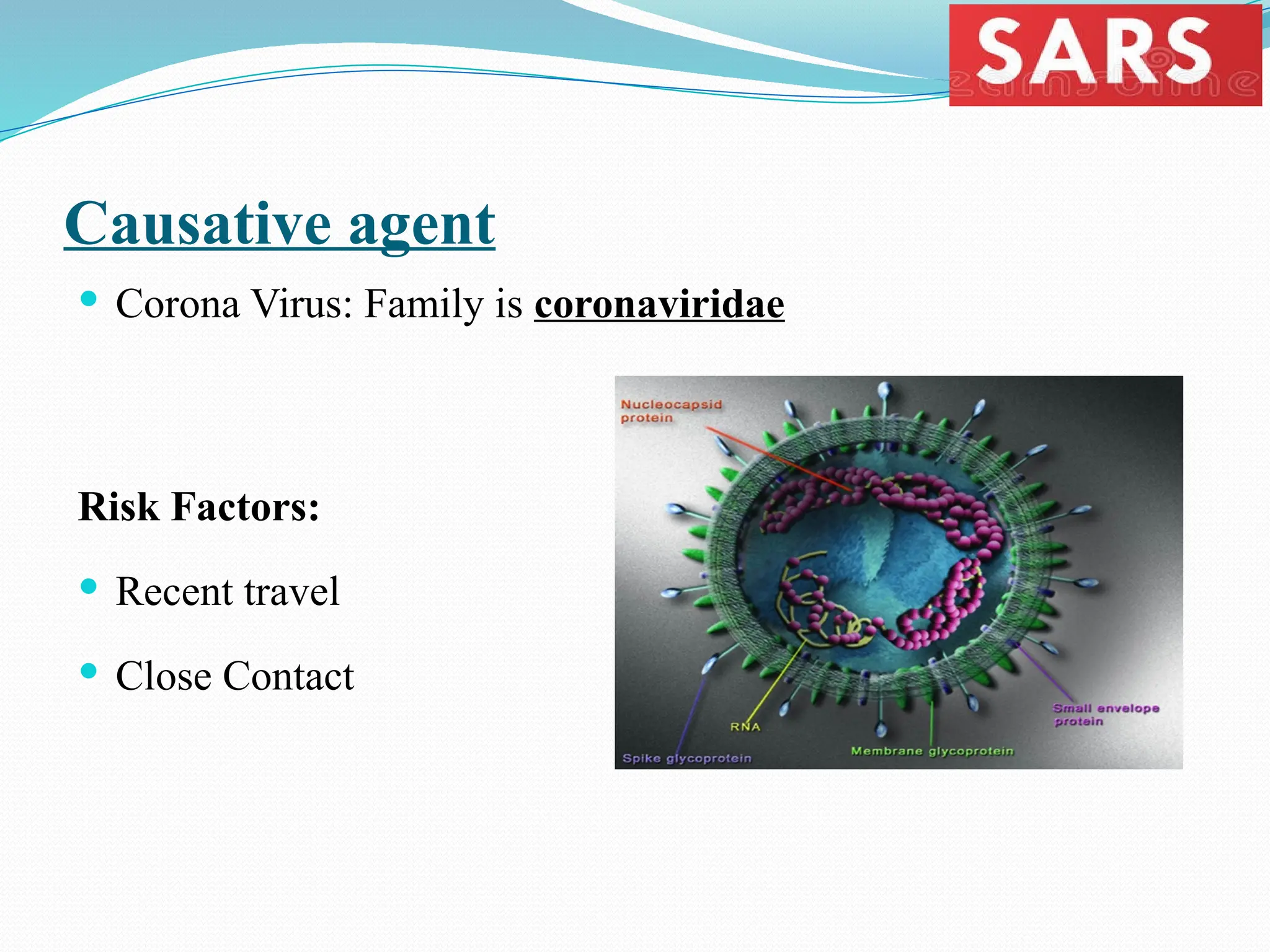
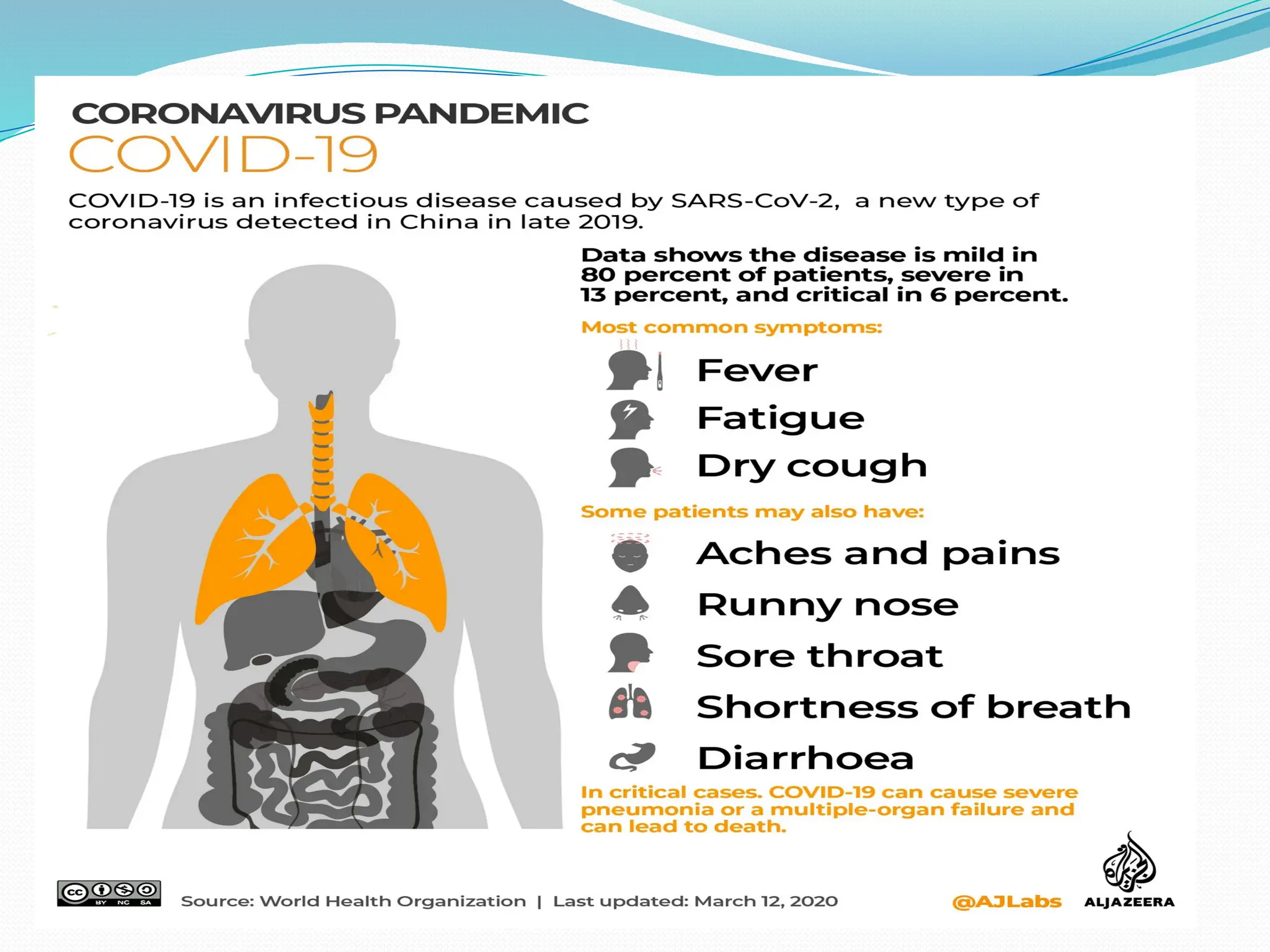
The document provides an overview of communicable diseases, detailing various types including tuberculosis, hepatitis, and acute diarrheal disease, along with their transmission modes, causes, symptoms, and treatments. It highlights the prevalence of these diseases in India and emphasizes the impact on the healthcare system while discussing potential preventive measures. It also outlines the specific characteristics of diseases like hepatitis and the measures available for control and vaccination.