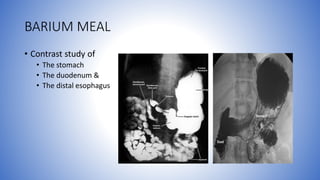
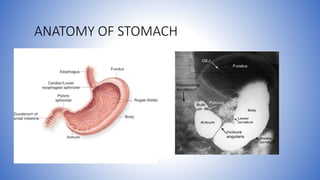
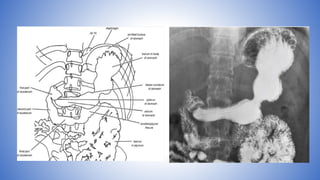
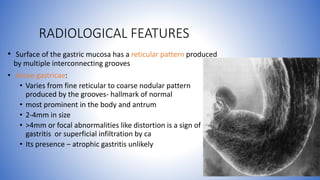
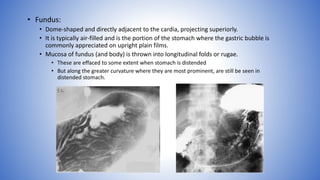
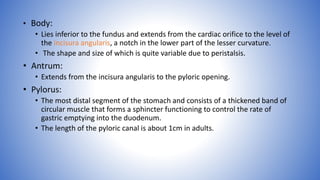
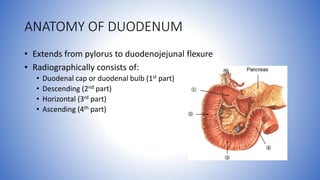
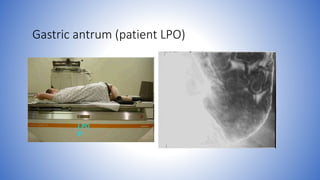
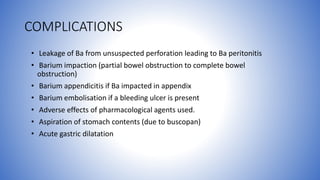
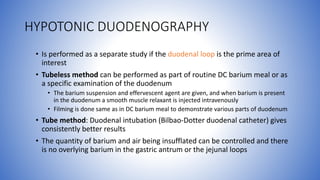
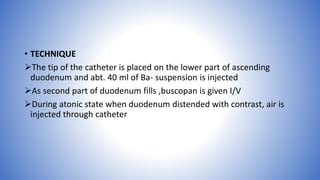
The document provides a comprehensive overview of barium meal studies, detailing the anatomy of the stomach and duodenum, radiological features, indications for the procedure, and various methods including single, double, and biphasic contrast studies. It also discusses contraindications, patient preparation, procedural techniques, and complications related to barium contrast studies. Additionally, special modifications for pediatric patients and those with specific medical conditions are included to enhance diagnostic accuracy.