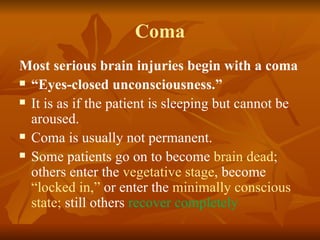
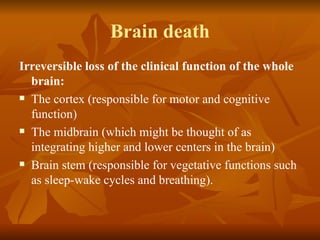
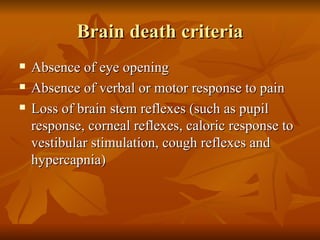
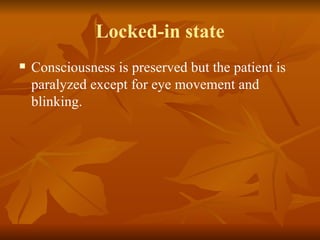
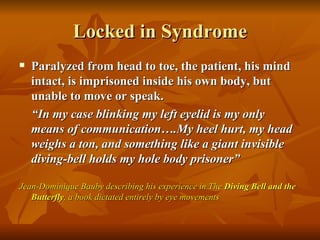
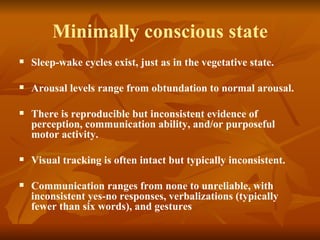
Brain death and ethical issues are discussed. Brain death refers to irreversible loss of function of the whole brain including the brain stem. It is diagnosed using criteria such as absence of brain stem reflexes. This is distinct from other conditions like coma, vegetative state, or locked-in syndrome. While brain death is accepted in Islam and Pakistan, legislation on it is lacking. Famous legal cases around withdrawing life support are discussed. Ethical issues arise around ceasing medical efforts for those who are brain dead.