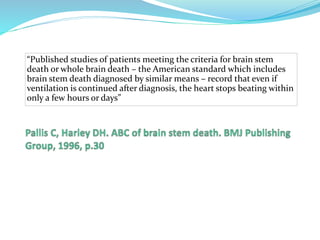
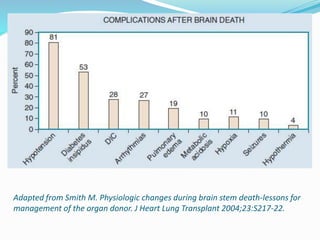
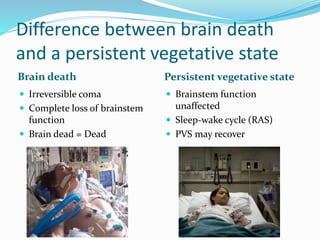
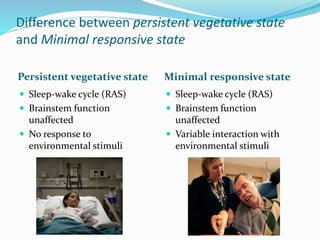
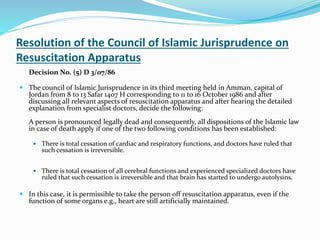
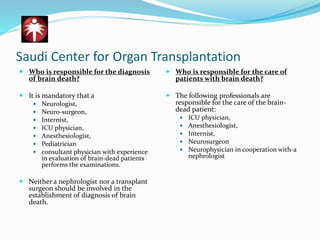
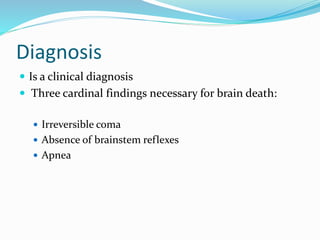
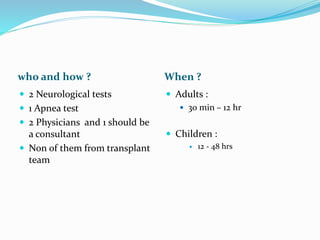
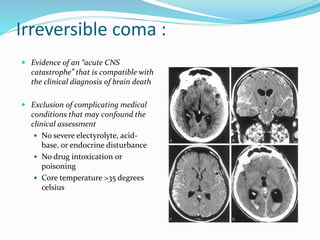
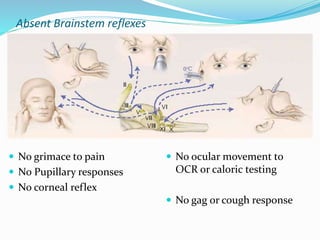
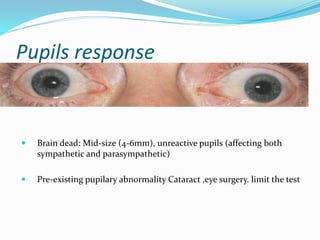
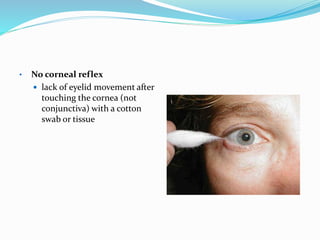
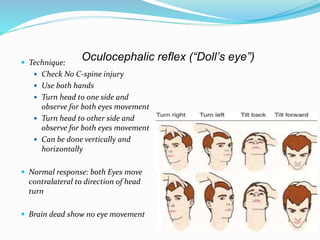
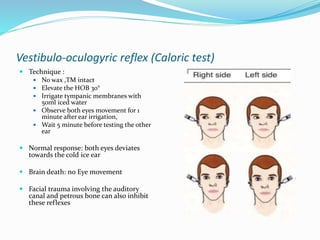
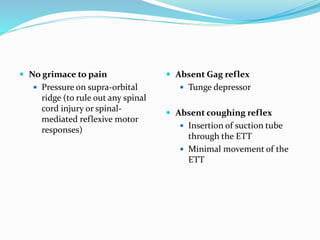
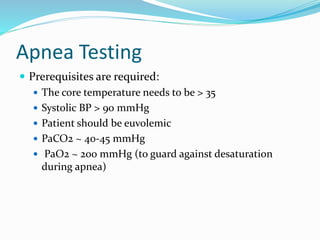
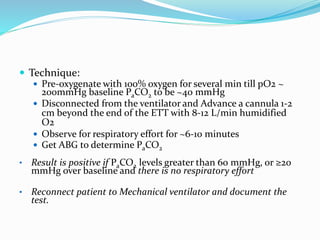
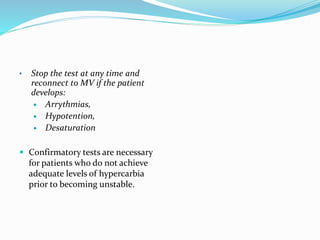
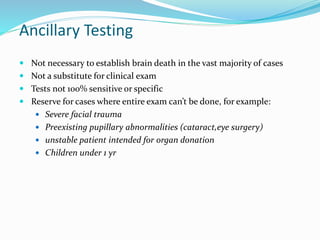
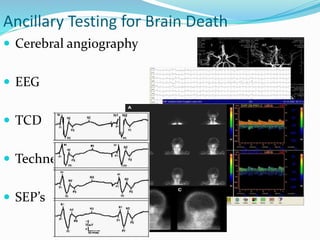
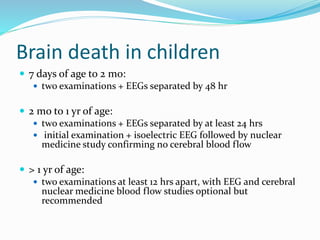
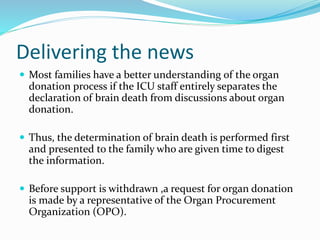
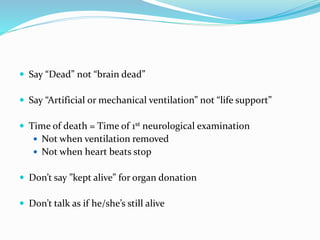
This document discusses brain death, its diagnosis, and organ donation. It provides definitions of brain death standards in the U.S. and U.K. Diagnosing brain death requires demonstrating irreversible loss of brain and brainstem functions through clinical exams and tests like apnea testing. Key findings that must be absent are brainstem reflexes, response to pain, and spontaneous breathing. The process of declaring brain death should be separate from discussing organ donation with family.