1) Brain death is the irreversible loss of all brain and brainstem functions and is diagnosed clinically through examination of coma, absent brainstem reflexes, and apnea on testing.
2) The role of the intensivist is to determine if the patient meets criteria for brain death through clinical examination and ancillary testing, and to prepare potential organ donors.
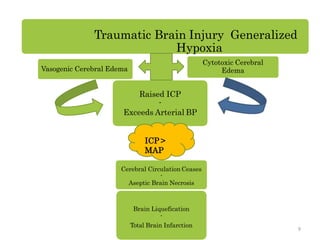
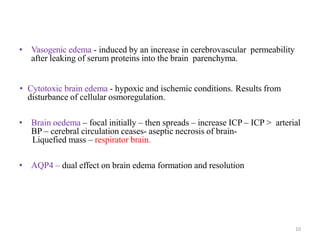
3) Brain death results from severe brain injury or lack of oxygen that causes raised intracranial pressure, cessation of cerebral blood flow, and ultimately complete necrosis of brain tissue.
![PUPILLARY REFLEX
• Absent pupillary reflex to
direct and consensual light
[cranial nerve II and III];
pupils need not be equal or
dilated.
• Conditions interfering in the
pupillary reflex are orbital
trauma, head injury, cataracts,
and medications like high dose
dopamine, glutethamide,
scopolamine, atropine,
bretylium or monoamine
oxidase inhibitors.
22](https://image.slidesharecdn.com/brainstemdeath3-210825173844/85/Brain-stem-death3-22-320.jpg)
![• Absent corneal reflex
[cranial nerve V and VII],
oculocephalic (also called
Doll eye movement), cough
and gag reflexes [cranial
nerve IX and X].
• The corneal reflex may be
altered as a result of facial
weakness
23](https://image.slidesharecdn.com/brainstemdeath3-210825173844/85/Brain-stem-death3-23-320.jpg)
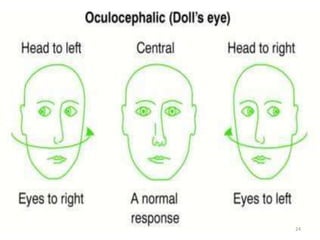
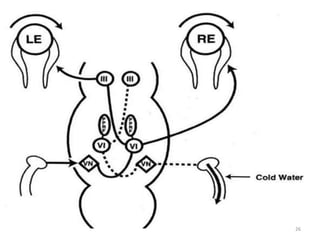
![Oculovestibular reflex
• Cold Caloric test /Absent oculovestibular reflex [cranial nerve VIII,
III and VI]:
• The external auditory canal should be clear of cerumen and
tympanic membranes should be intact.
• Elevate the patient‟s head by 30˚.
• Twenty to fifty (20 to 50) ml of ice water irrigated into external
auditory canal and over the tympanic membrane using a soft
irrigation cannula.
• One should look for eye ball movement for which upper eyelids
need to be retracted.
• Allow 1 minute response time after injection/irrigation of fluid and
at least 5 minutes between testing on each side.
• No eye ball movements will be seen in brain dead patient.
25](https://image.slidesharecdn.com/brainstemdeath3-210825173844/85/Brain-stem-death3-25-320.jpg)