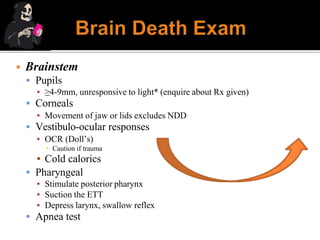
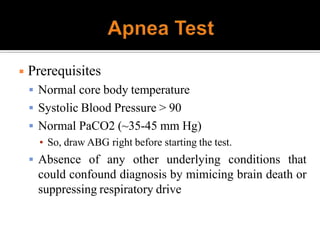
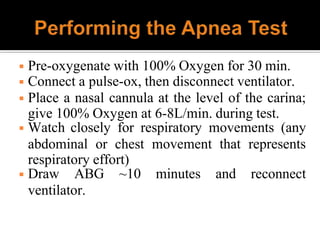
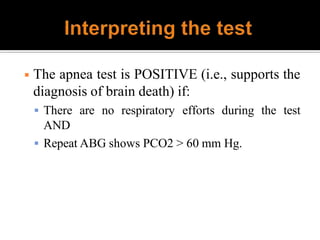
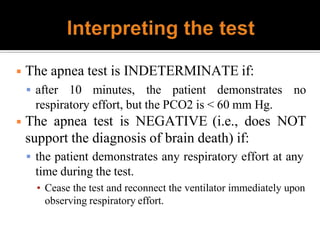
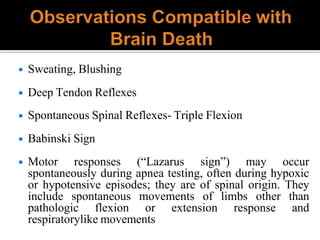
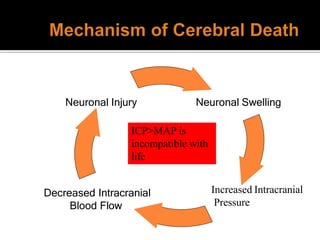
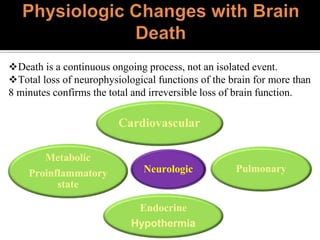
1) Brain death is defined as irreversible cessation of all functions of the entire brain, including the brainstem. Tests to determine brain death include examining brainstem reflexes and performing an apnea test.
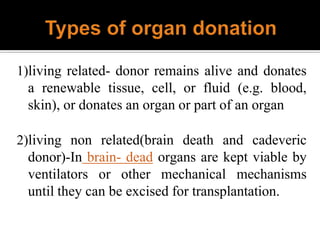
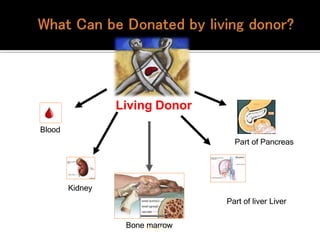
2) Organ donation provides terminally ill patients a new lease on life but organ availability is low in India. Living donors can donate renewable tissues while deceased donors are a major source of organs.
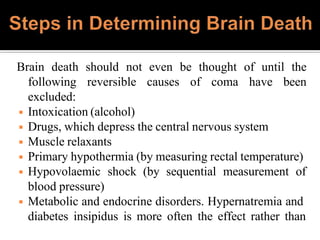
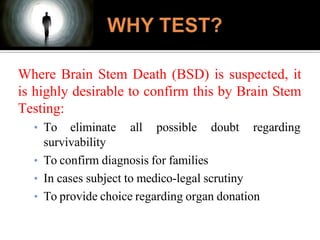
3) For organ donation to occur, all reversible causes of coma must first be excluded through testing and the diagnosis of brain death must be certified by a board of medical experts according to the law.

![In India, according to the Transplantation of Human Organs Act
[TOHO 1994 (Sub section 6 of Section 3)], “Brainstem death”
means the stage at which all functions of the brainstem have
permanently and irreversibly ceased and is so certified by a
“Board of Medical Experts” consisting of:
◾ The Medical Superintendent (MS) in charge of the hospital in
which “brainstem” death has occurred.
◾ A specialist, nominated by the MS in charge of the hospital, from
a panel of names approved by the Appropriate Authority.
◾ A neurologist or neurosurgeon, nominated by the MS in charge of
the hospital, from a panel of names approved by the appropriate
authority.](https://image.slidesharecdn.com/aayushppt-230823161600-b2c4ca8d/85/AAYUSH-PPT-pptx-6-320.jpg)