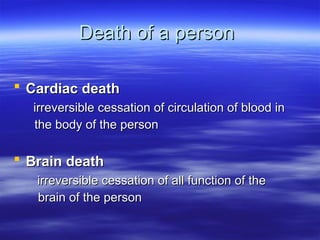
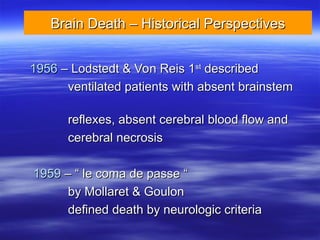
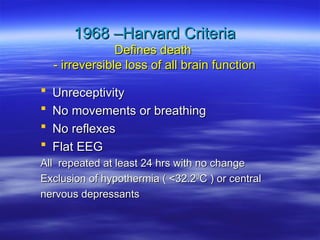
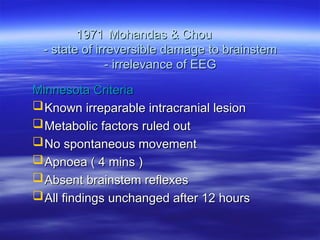
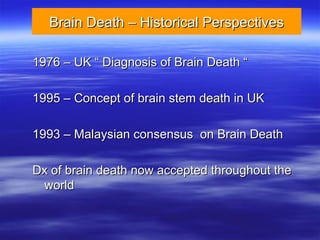
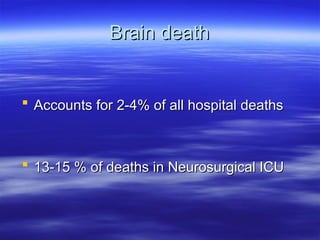
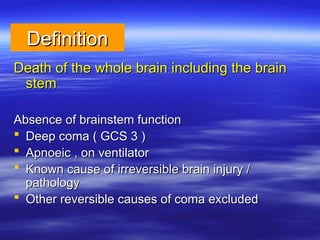
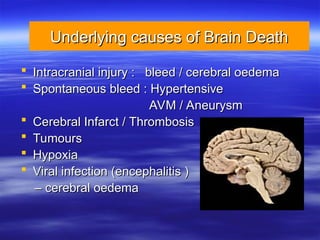
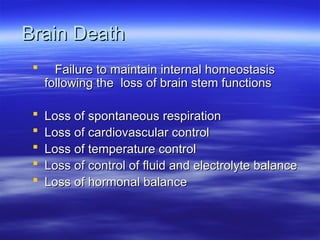
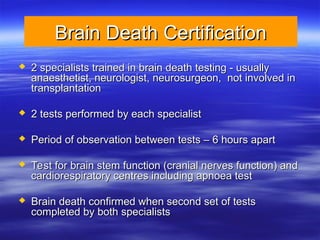
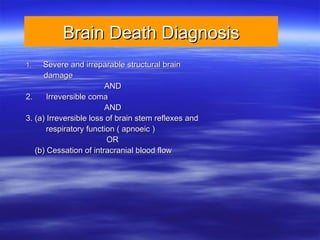
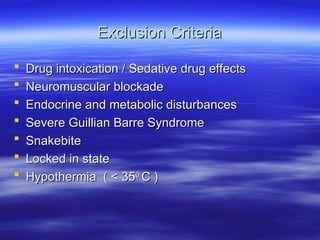
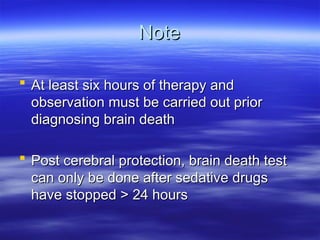
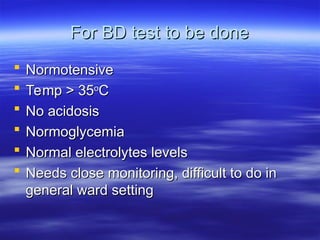
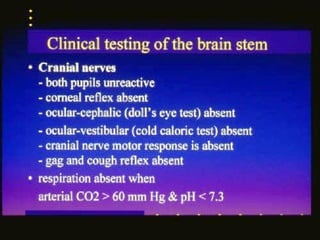
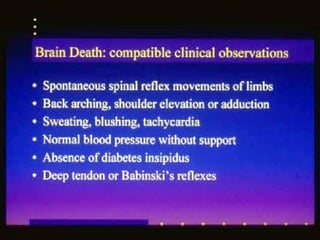
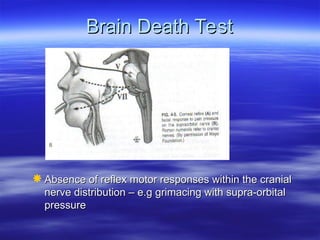
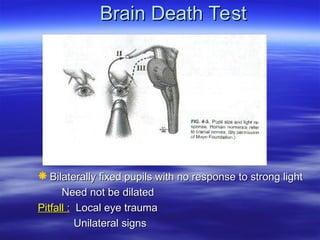
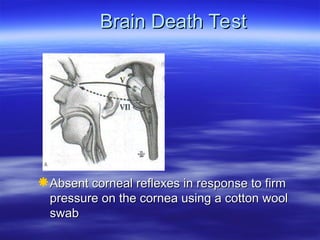
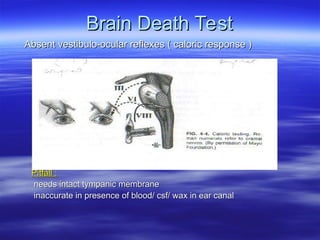
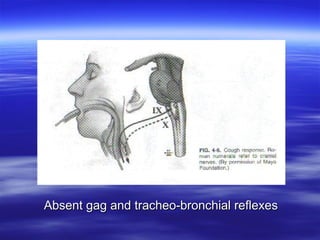
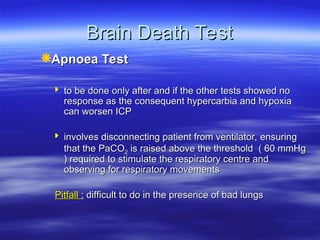
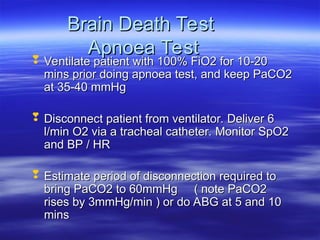
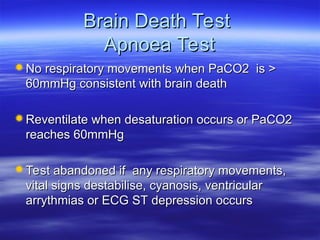
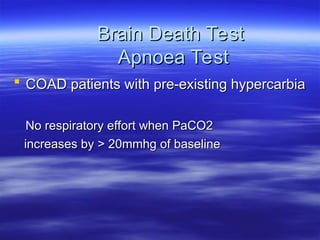
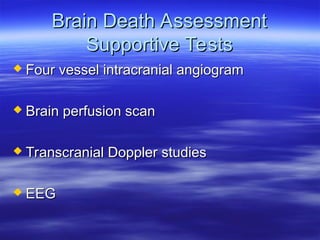
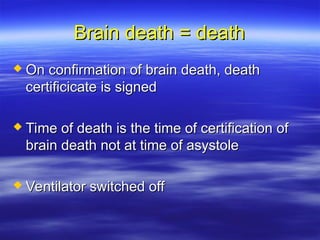
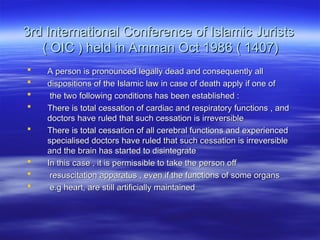
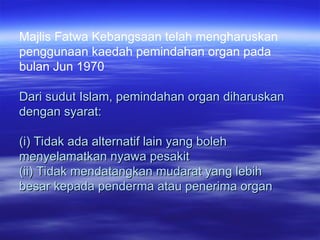
The document discusses the definition and criteria for brain death, highlighting historical perspectives and diagnostic processes. It outlines the physiological criteria for confirming brain death, the role of specialists in diagnosis, and the ethical considerations surrounding organ donation. Brain death is presented as a legally recognized condition that leads to the cessation of all functions of the brain, with relevant diagnostic tests and exclusion criteria detailed for assessment.