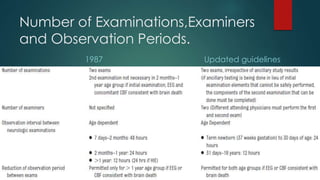
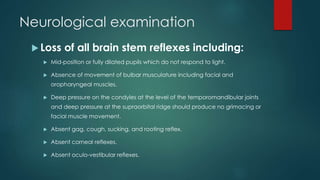
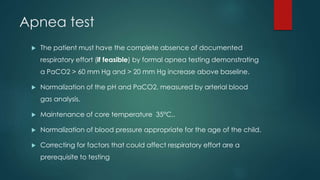
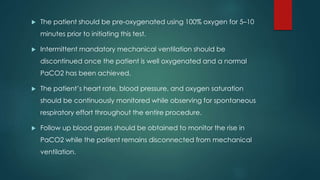
Brain death is a clinical diagnosis based on the absence of neurologic function and irreversible coma. A complete neurologic examination is required to determine brain death, which must show no brainstem reflexes, no response to stimuli, apnea on testing, and flaccid muscle tone. Ancillary tests like EEG or angiography can assist in diagnosis but are not required. Special considerations are needed for diagnosing brain death in newborns and preterm infants due to the potential for reversible conditions and lack of brain development. Death is declared after two examinations show no changes confirming an irreversible condition.