This document discusses brain death and the determination of brain death. It provides:
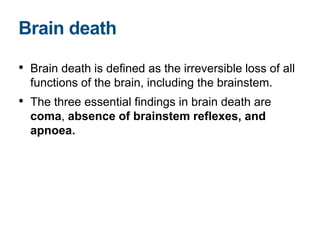
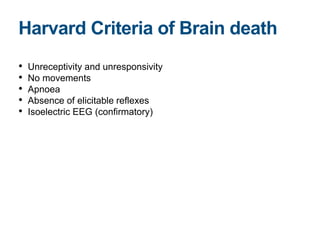
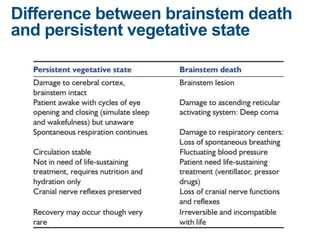
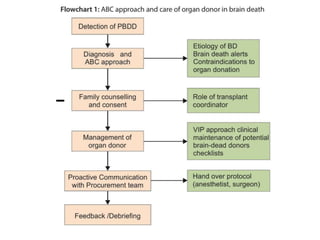
1) A definition of brain death as the irreversible loss of all functions of the brain, including the brainstem, as evidenced by coma, absence of brainstem reflexes, and apnoea.
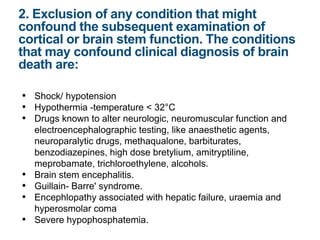
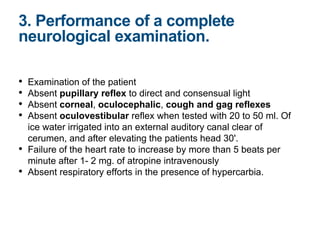
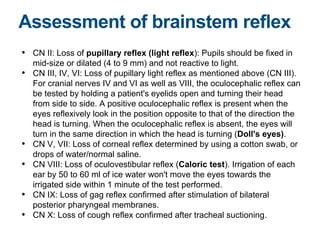
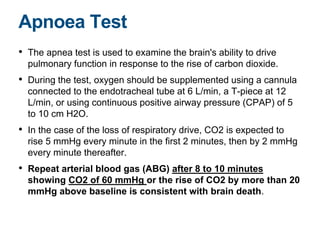
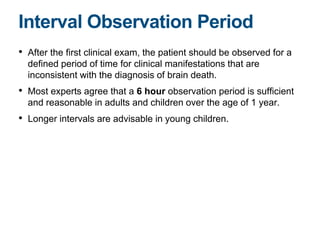
2) Details the clinical criteria for determining brain death, including neurological examination to check for absence of brainstem reflexes and an apnoea test.
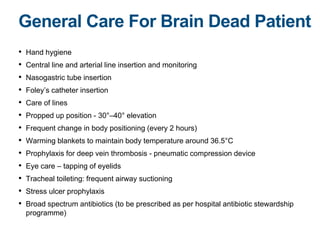
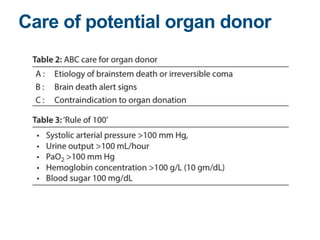
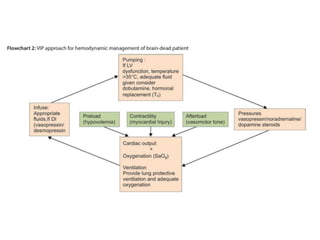
3) Outlines the general care and management of a potential organ donor who is brain dead, including maintaining body temperature and position, treating for infections, and eye and airway care.