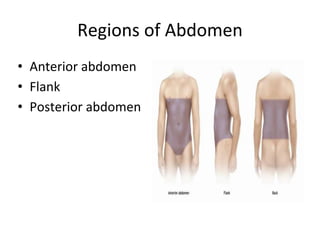
This document provides an overview of the types, causes, examination, and management of abdominal trauma from blunt forces. It discusses the different regions of the abdomen that can be injured and mechanisms of injury for hollow and solid organs. Specific injuries to the spleen, liver, pancreas, kidneys, diaphragm, stomach, duodenum, intestines, colon, and bladder are reviewed. Management approaches for stable and unstable patients are described, including non-operative management with monitoring versus exploratory surgery depending on injury grade and hemodynamic status. Imaging tools like ultrasound, CT scan, and diagnostic peritoneal lavage are also summarized.