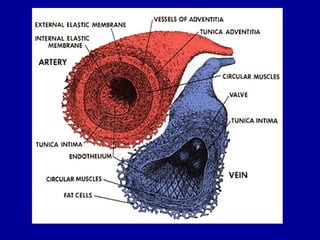
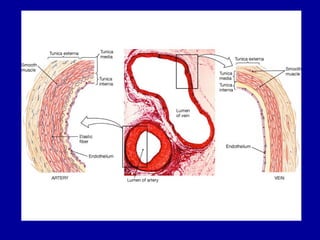
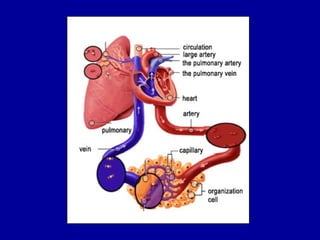
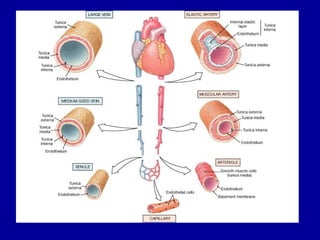
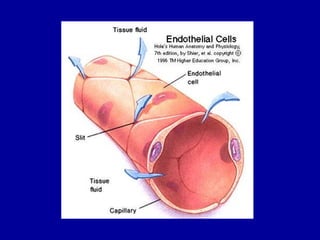
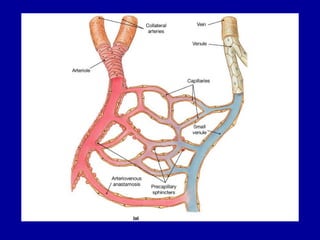
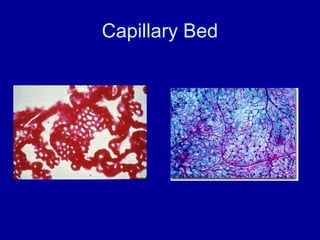
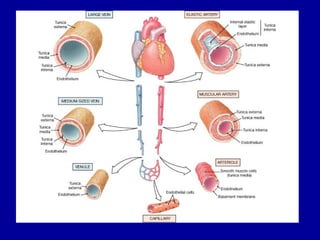
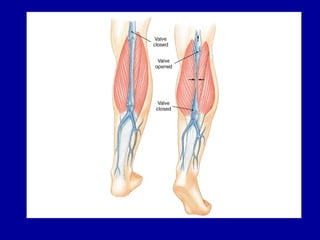
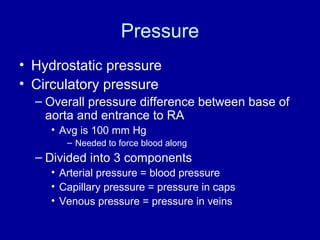
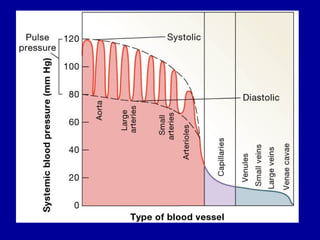
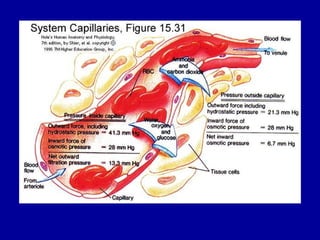
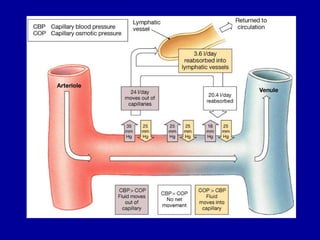
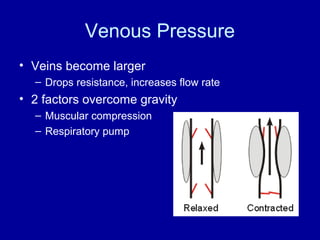
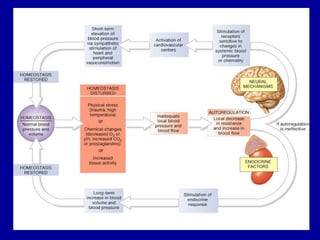
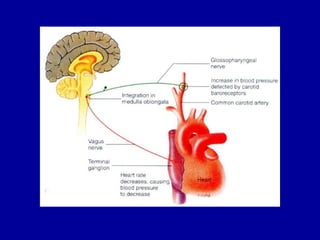
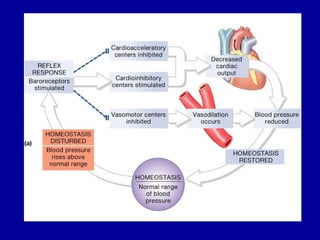
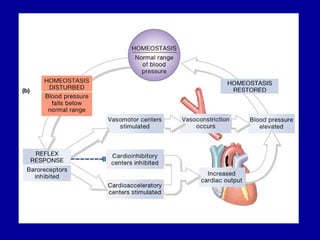
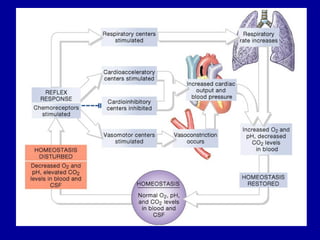
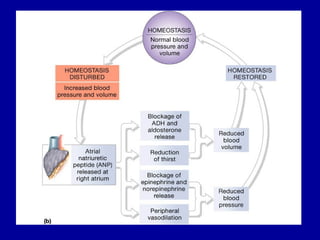
Blood vessels transport blood throughout the body. There are three main types: arteries, which carry blood away from the heart; capillaries, where nutrients and wastes are exchanged; and veins, which carry blood back to the heart. Blood flow is regulated through pressure, resistance, and the actions of the cardiovascular system to ensure adequate circulation throughout the body. Neural and hormonal mechanisms precisely control blood pressure and flow through reflexes and the release of substances like epinephrine and norepinephrine.