This document provides a summary of key information about blood:
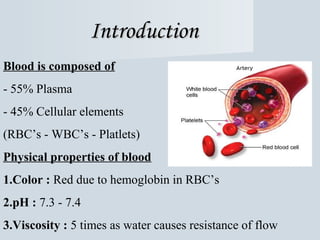
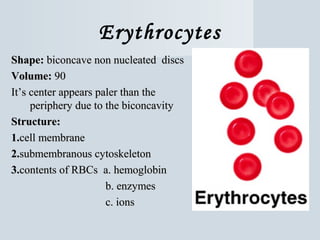
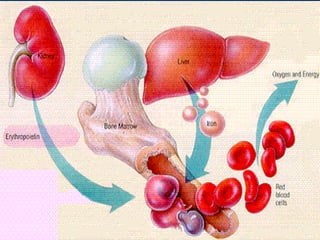
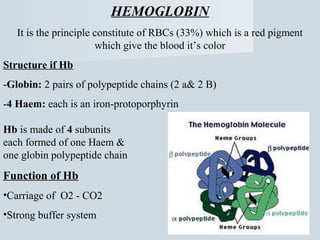
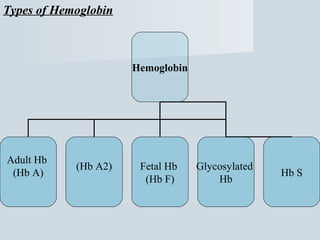
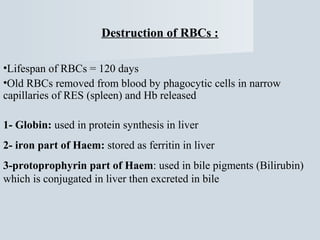
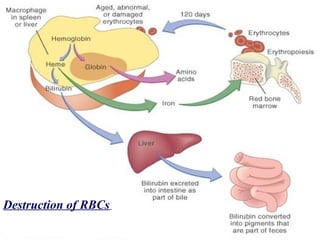
1. Blood is composed of plasma and cellular elements including red blood cells, white blood cells, and platelets. Red blood cells contain hemoglobin which gives blood its red color and allows it to carry oxygen.
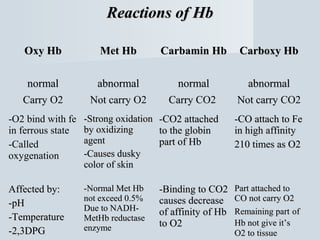
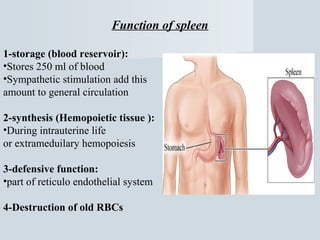
2. The main functions of blood are to transport oxygen, carbon dioxide, nutrients, hormones and waste products throughout the body, to fight infections through white blood cells, and to regulate pH, temperature, water content and pressure.
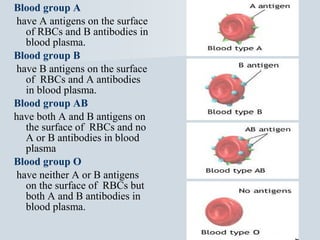
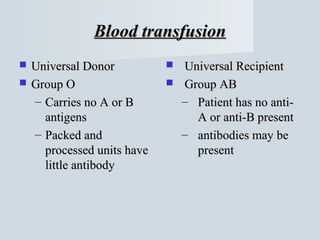
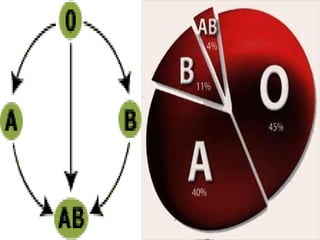
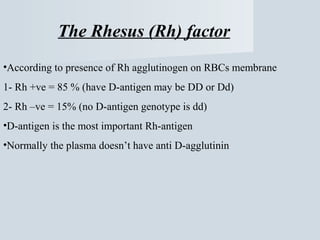
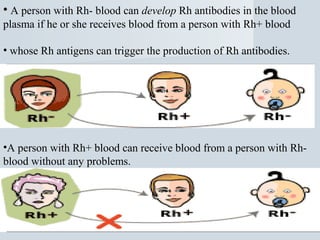
3. Blood groups are classified by the presence or absence of antigens on red blood cells. The main blood group systems are ABO and Rh factor. Compatible blood types are required for safe blood transfusions.
![بسم ال الرحمن الرحيم
]البقرة :23[](https://image.slidesharecdn.com/bloodppta-140309203103-phpapp01/75/Blood-Overview-PPT-1-2048.jpg)