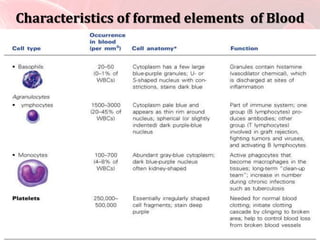
Blood transports nutrients, oxygen, waste, and immune cells throughout the body. It contains plasma and formed elements including red blood cells, white blood cells, and platelets. Red blood cells carry oxygen via hemoglobin while white blood cells help fight infection. Platelets assist in clotting to prevent blood loss from injuries. There are several blood types defined by antigens on red blood cells, and compatibility of antigens is important for safe blood transfusions.