The document discusses the anatomy and diseases of the gallbladder and bile ducts. It provides details on:
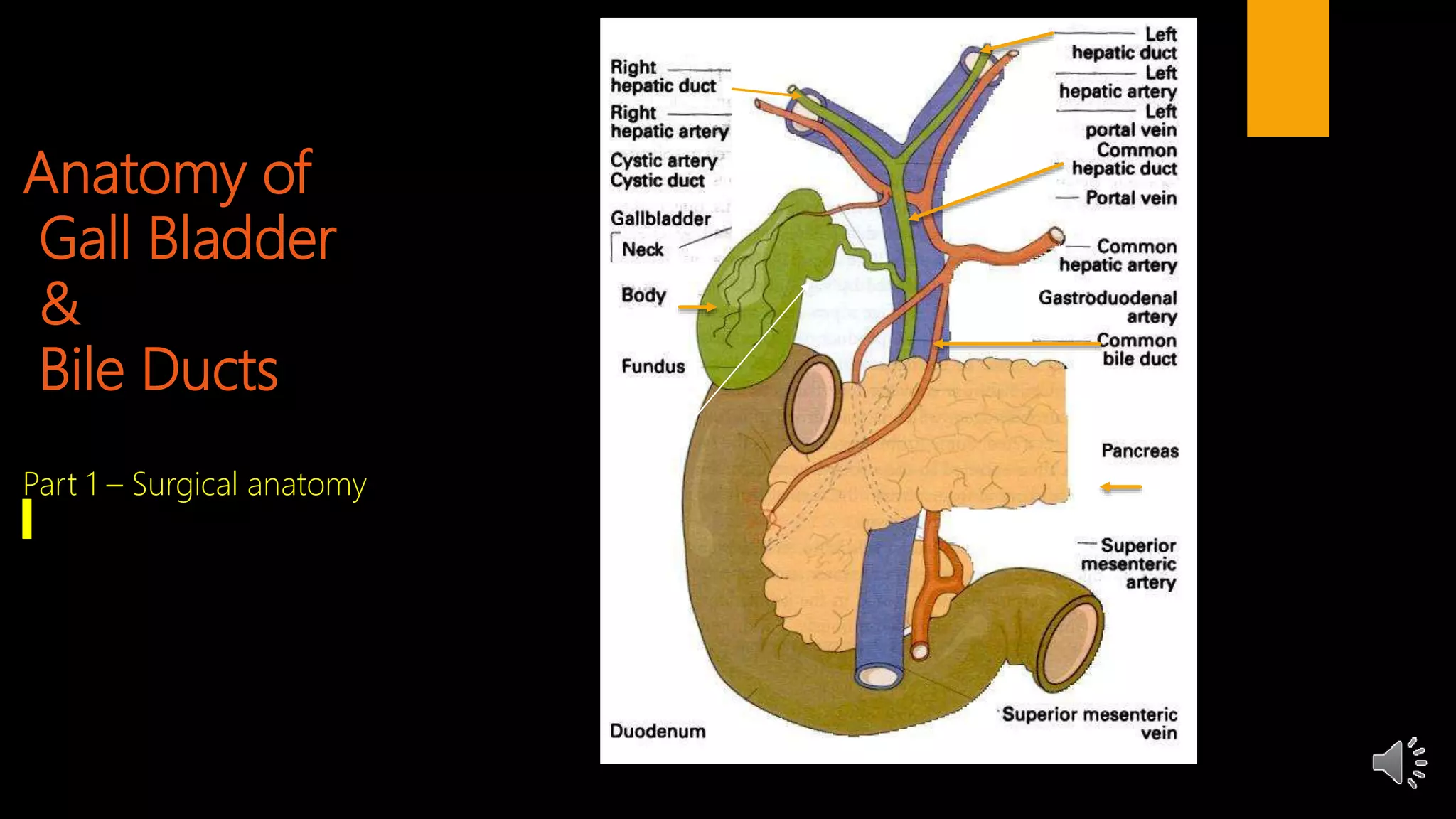
1. The anatomy of the gallbladder, cystic duct, common bile duct, and sphincter of Oddi.
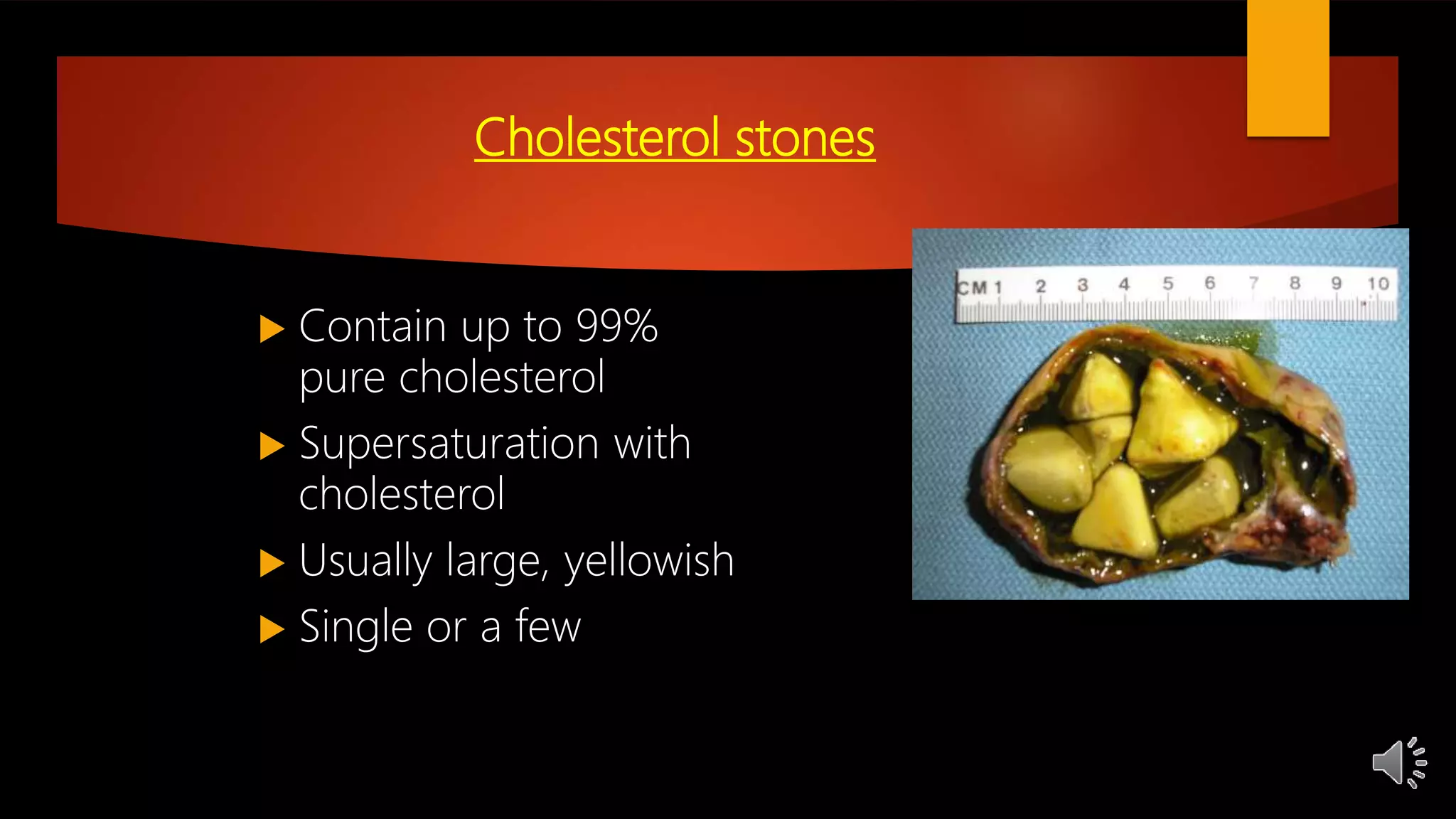
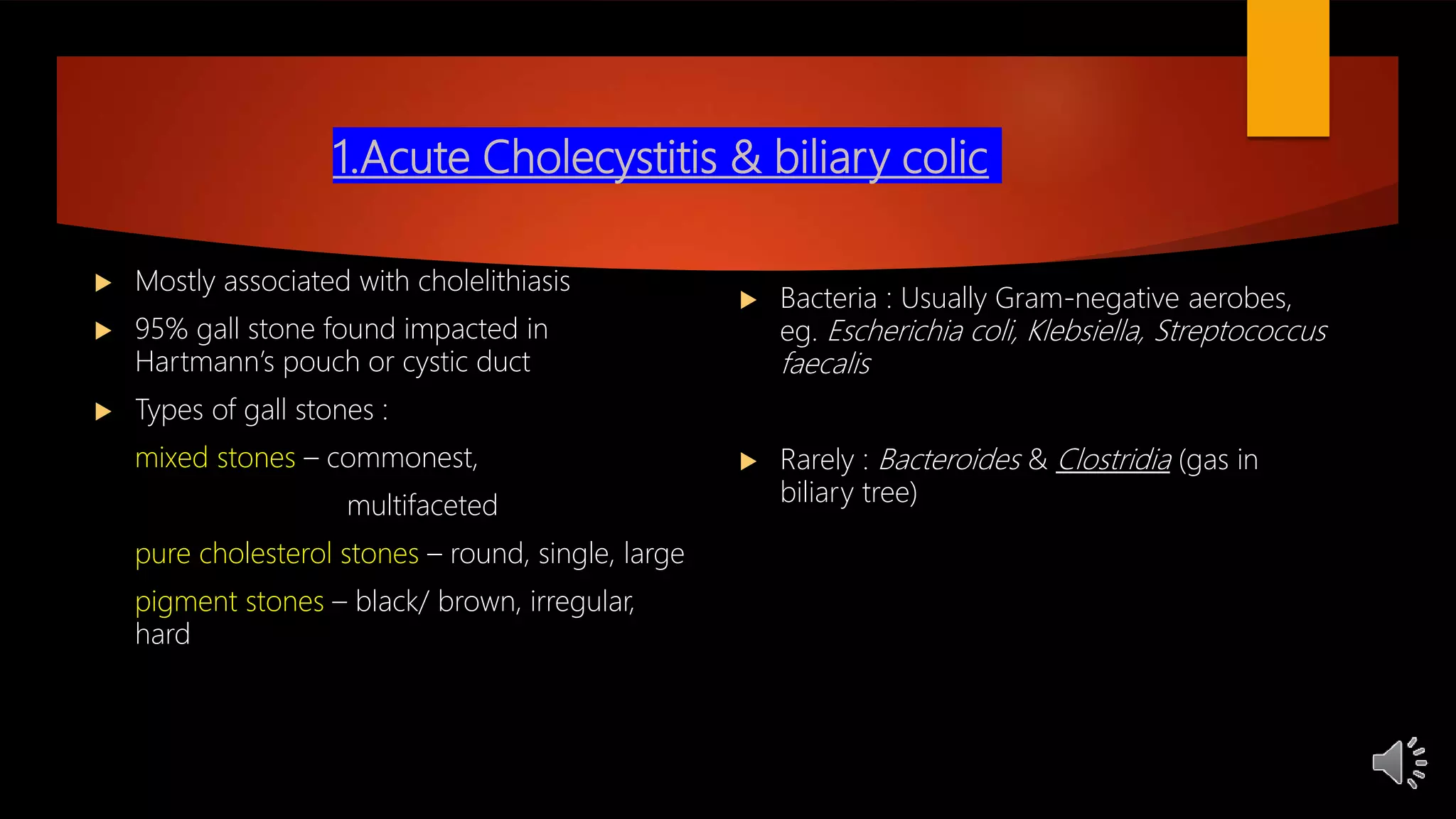
2. Common gallbladder and bile duct diseases including gallstones, cholecystitis, cholangitis, strictures, cancers, and more.
3. The symptoms, signs, investigations, and treatments for various diseases like acute cholecystitis, chronic cholecystitis, and bile duct stones.
Cholecystectomy is often the treatment for gallbladder diseases while bile duct diseases may require other interventions. A thorough understanding of the anatomy and diseases is