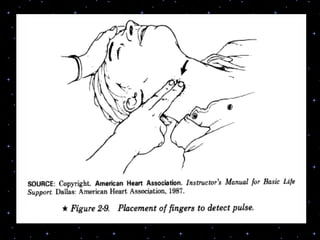
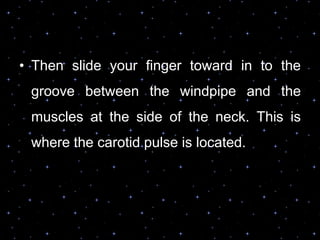
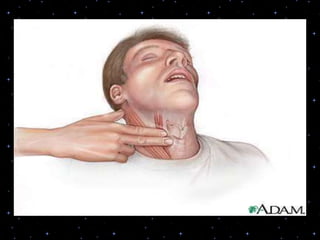
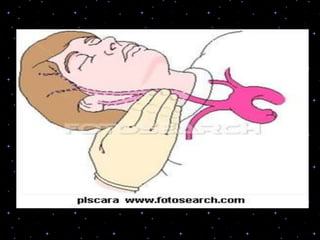
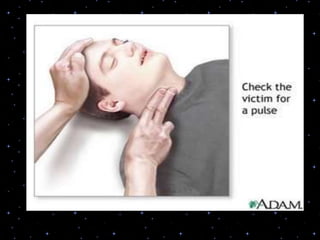
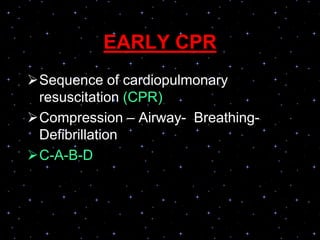
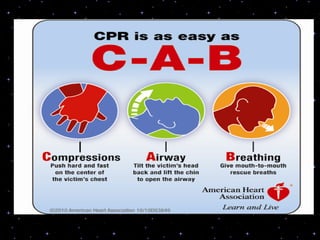
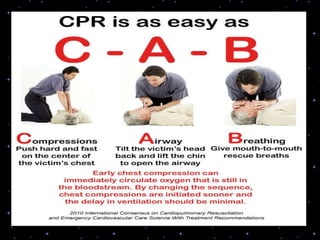
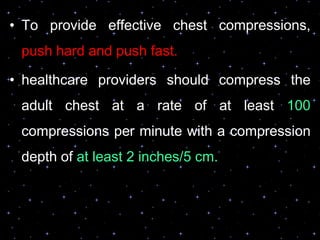
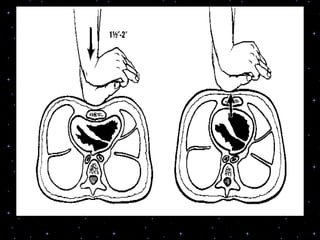
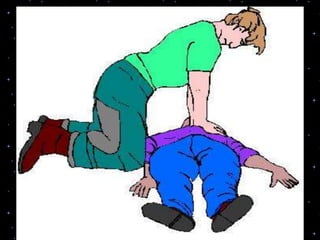
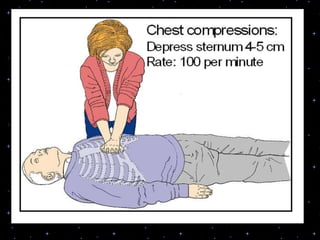
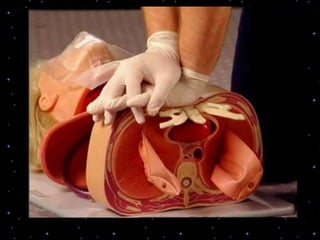
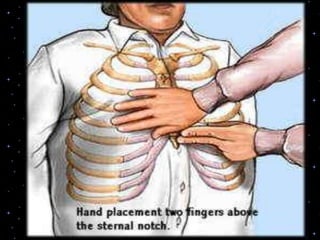
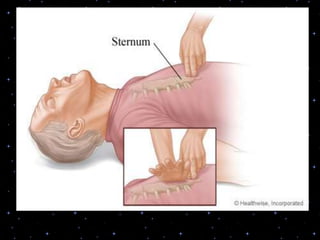
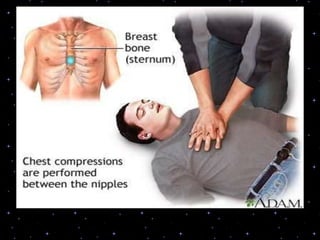
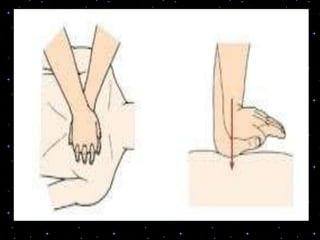
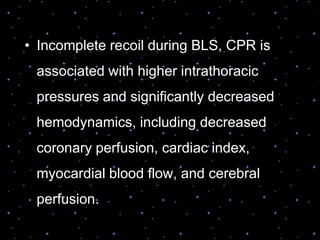
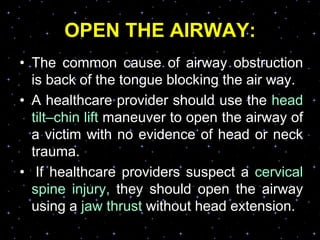
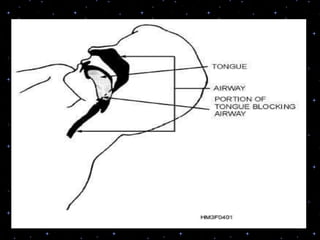
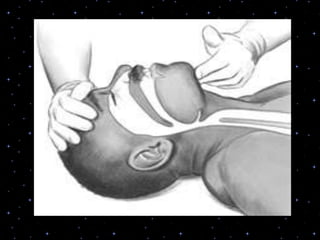
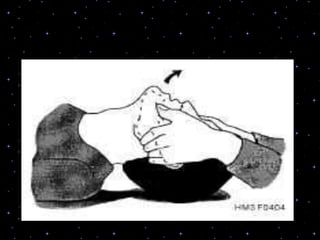
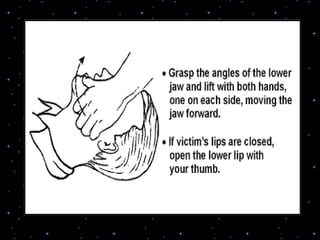
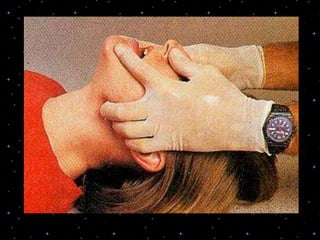
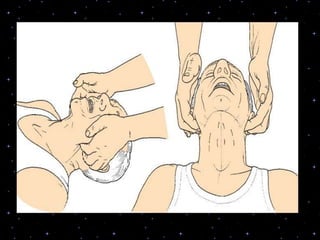
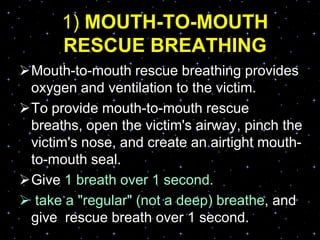
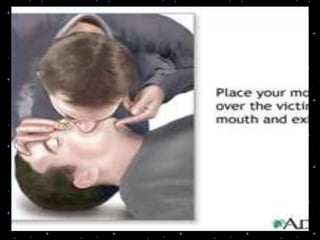
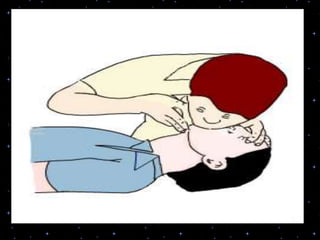
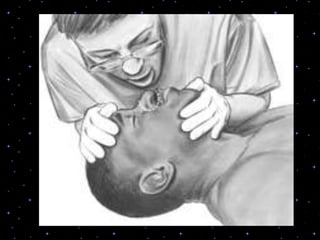
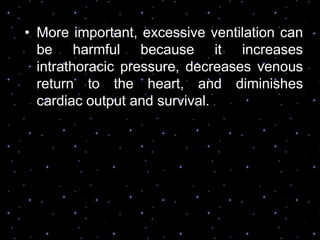
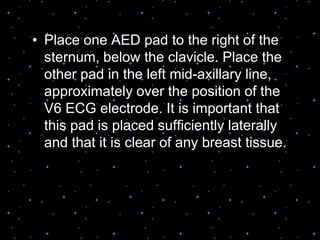
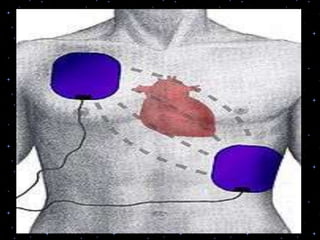
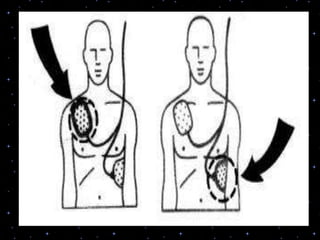
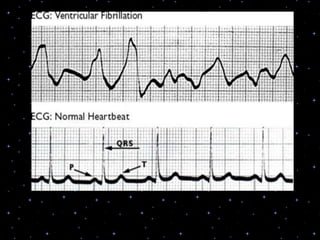
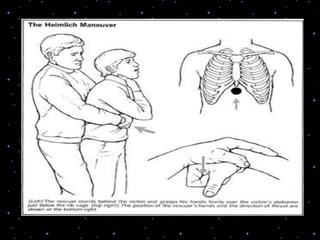
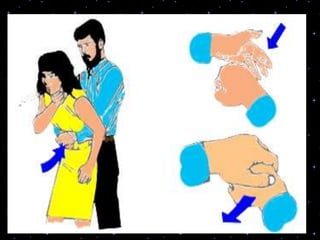
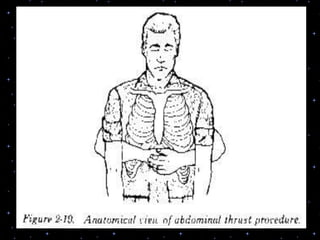
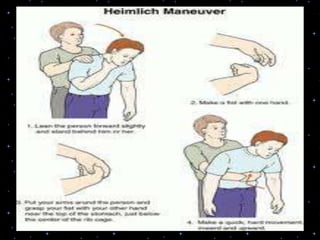
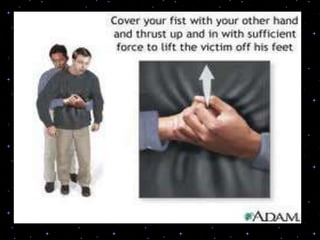
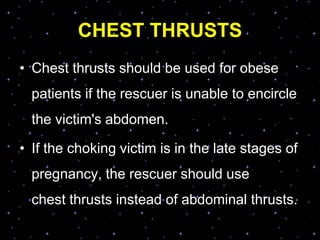
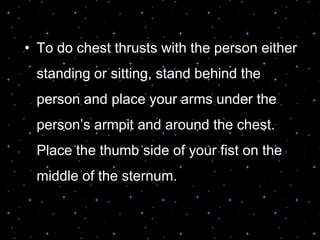
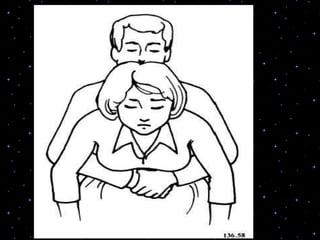
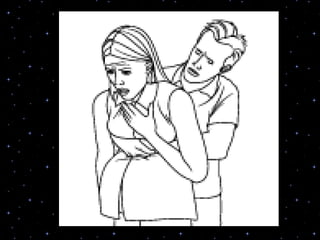
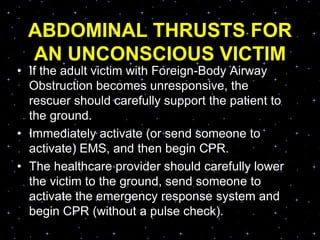
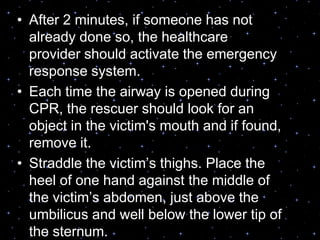
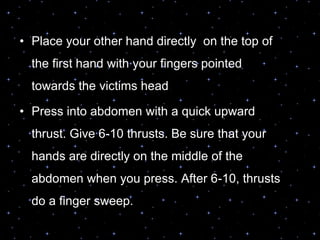
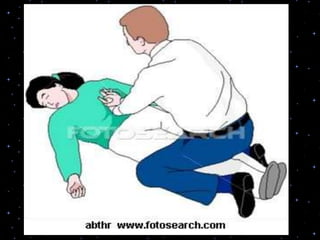
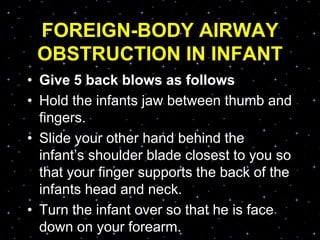
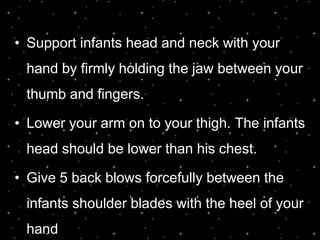
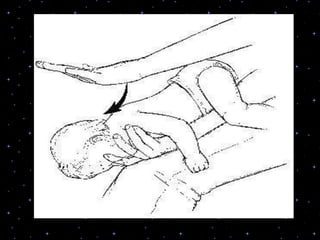
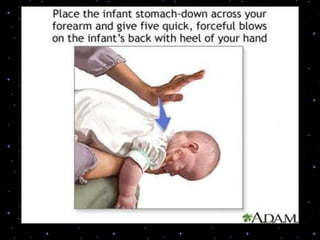
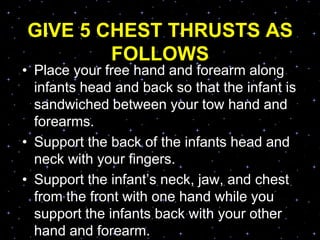
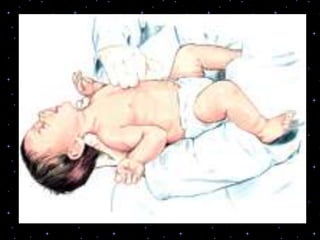
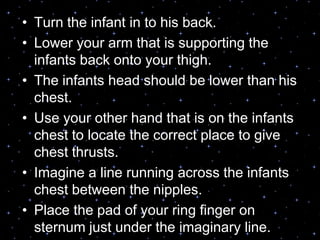
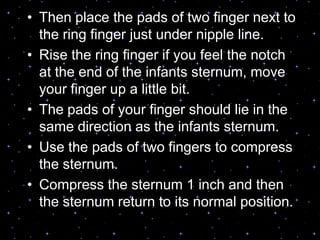
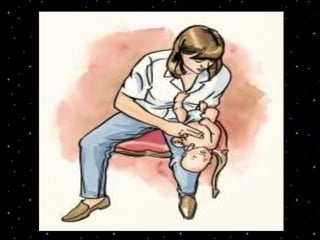
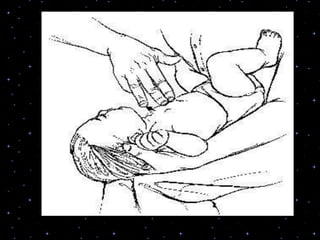
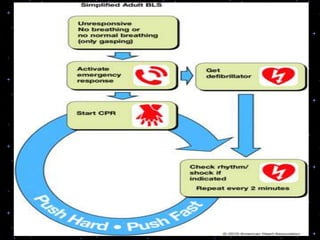
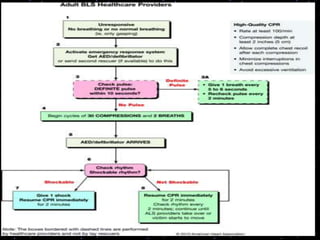
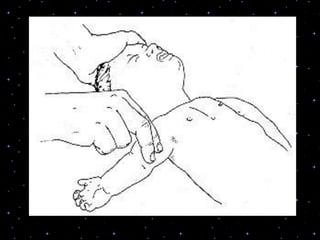
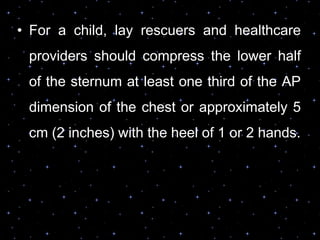
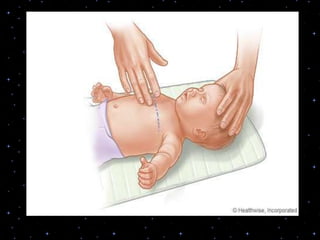
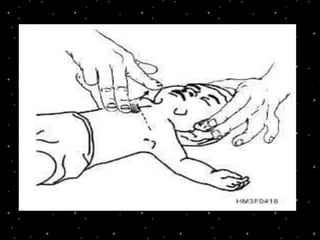
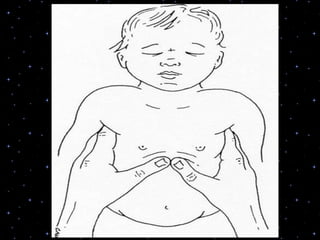
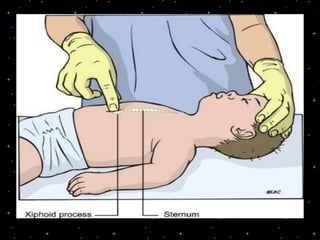
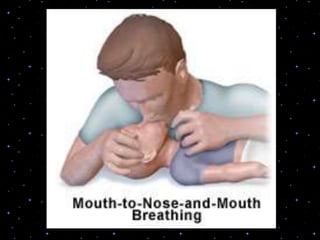
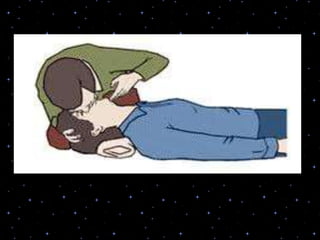
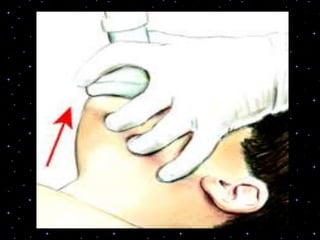
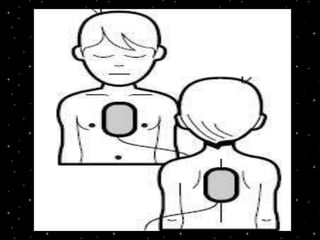
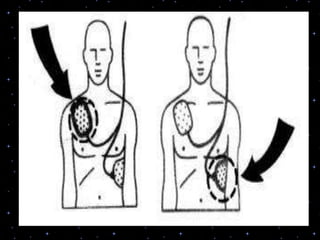
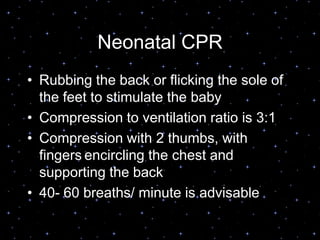
This document provides information on basic life support (BLS) procedures. It begins with an introduction to BLS, which includes immediate recognition of cardiac arrest, activation of emergency services, early CPR, and use of an automated external defibrillator. It then defines BLS and outlines the emergency action principle of assessing safety, doing a primary survey of the victim, activating EMS, and conducting a secondary assessment. The document provides detailed steps for conducting CPR, including chest compressions, opening the airway, giving rescue breaths, and using an AED. It also covers foreign body airway obstruction and procedures for infants.