Dysautonomia refers to a malfunction of the autonomic nervous system that controls involuntary body functions like heart rate, blood pressure, digestion, and sweating. The document discusses the anatomy and functions of the autonomic nervous system and its divisions. It then defines dysautonomia and lists various causes like diabetes, multiple sclerosis, and injuries. Common symptoms involve fatigue, dizziness, digestive issues, urinary problems, and temperature regulation difficulties. Tests of autonomic function are described that measure responses like heart rate and blood pressure during maneuvers to identify autonomic dysfunction.
![CAUSES
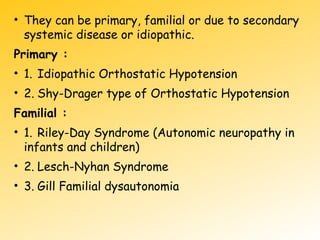
• Dysautonomia may be due to inherited or
degenerative neurological disorders[primary
dusautonomia] or may be due to injury of ANS
due to an acquired disorder[secondary
dysautonomia
• Side effects of some drugs can cause
abnormalities in the function of
ANS,producing an iatrogenic form of
dysautonomia](https://image.slidesharecdn.com/dysautonomia-160405193307/85/Dysautonomia-21-320.jpg)
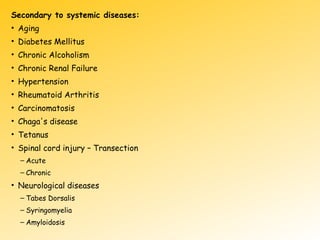
![.
• Diabetes mellitus
• Multiple sclerosis
• Parkinson’s disease
• HIV and AIDS
• Amyloidosis
• Boutilism
• Pure autonomic failure
• Lyme disease amd Tuberculosis
• Lupus,Sjogen’s syndrome,sarcodiasis[A-I disorders]
• Chronic alcohol misuse
• Spinal cord injury
• Physical trauma or injury](https://image.slidesharecdn.com/dysautonomia-160405193307/85/Dysautonomia-22-320.jpg)
![Indications for ANS testing
• Syncope[sudden loss of consciousness]
• Central autonomic degeneration ex. Parkinsons
• Pure autonomic failure
• Postural tachycardia syndrome
• Autonomic and small fiber peripheral neuropathies ex.-
diabetic neuropathy
• Sympathetically mediated pain
• Evaluating response to therapy
• Differentiating benign symptoms from autonomic
disorders](https://image.slidesharecdn.com/dysautonomia-160405193307/85/Dysautonomia-26-320.jpg)