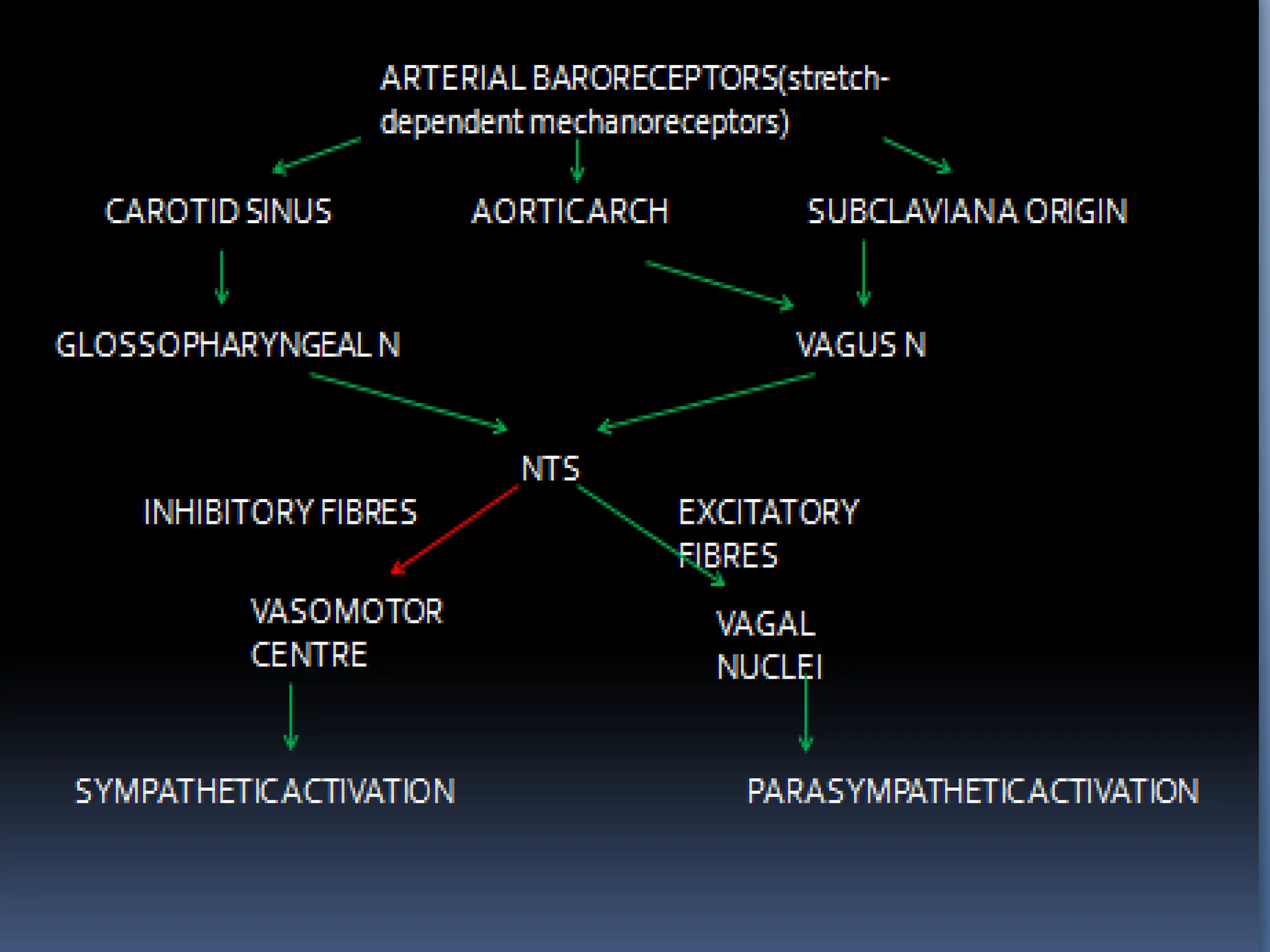
This document discusses the anatomy and physiology of the cardiac autonomic nervous system. It covers the extrinsic and intrinsic innervation of the heart, including the sympathetic and parasympathetic fibers. Evaluation methods for the autonomic system are described, such as orthostatic tests, heart rate variability, and tilt-table testing. Conditions related to autonomic dysfunction like postural orthostatic tachycardia syndrome and neurally mediated syncope are explained. The role of the autonomic system in arrhythmias and other cardiac conditions is also summarized.













































































![Safety and Efficacy of Renal Denervation as a Novel
Treatment for Ventricular Tachycardia Storm in Patients
with Cardiomyopathy
Remo et al ,Heart rhythm 2014
• Largest case series to date using RDN as adjunctive therapy for
refractory VT in patients with underlying cardiomyopathy
• 4 patients with recurrent VT despite maximal antiarrhythmics
and prior ablations
• The number of VT episodes was decreased from 11.0 ± 4.2
[5.0-14.0] during the month prior to the ablation to 0.3 ± 0.1
[0.2-0.4] per month after the ablation. All VT episodes occurred
in the first four months after ablation (2.6 ± 1.5 months).
• RDN was well tolerated acutely and demonstrated no clinically
significant complications during 8.8 ± 2.6 [5.0-11.0] months
follow-up](https://image.slidesharecdn.com/cardiacautonomicsystemclinicalsignificance-231106023625-e95ada7f/75/CARDIAC-AUTONOMIC-SYSTEM-CLINICAL-SIGNIFICANCE-pptx-83-2048.jpg)


































