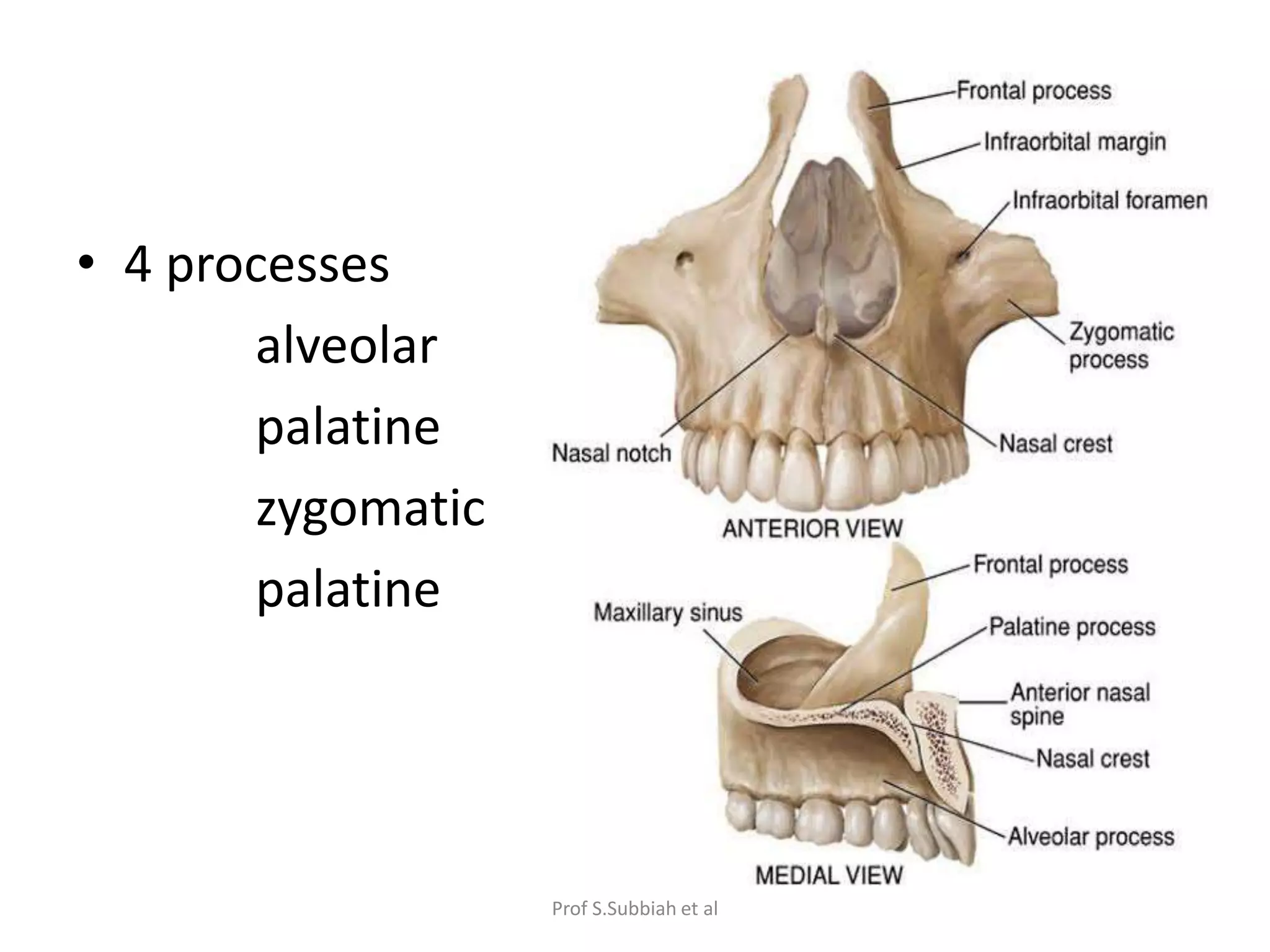
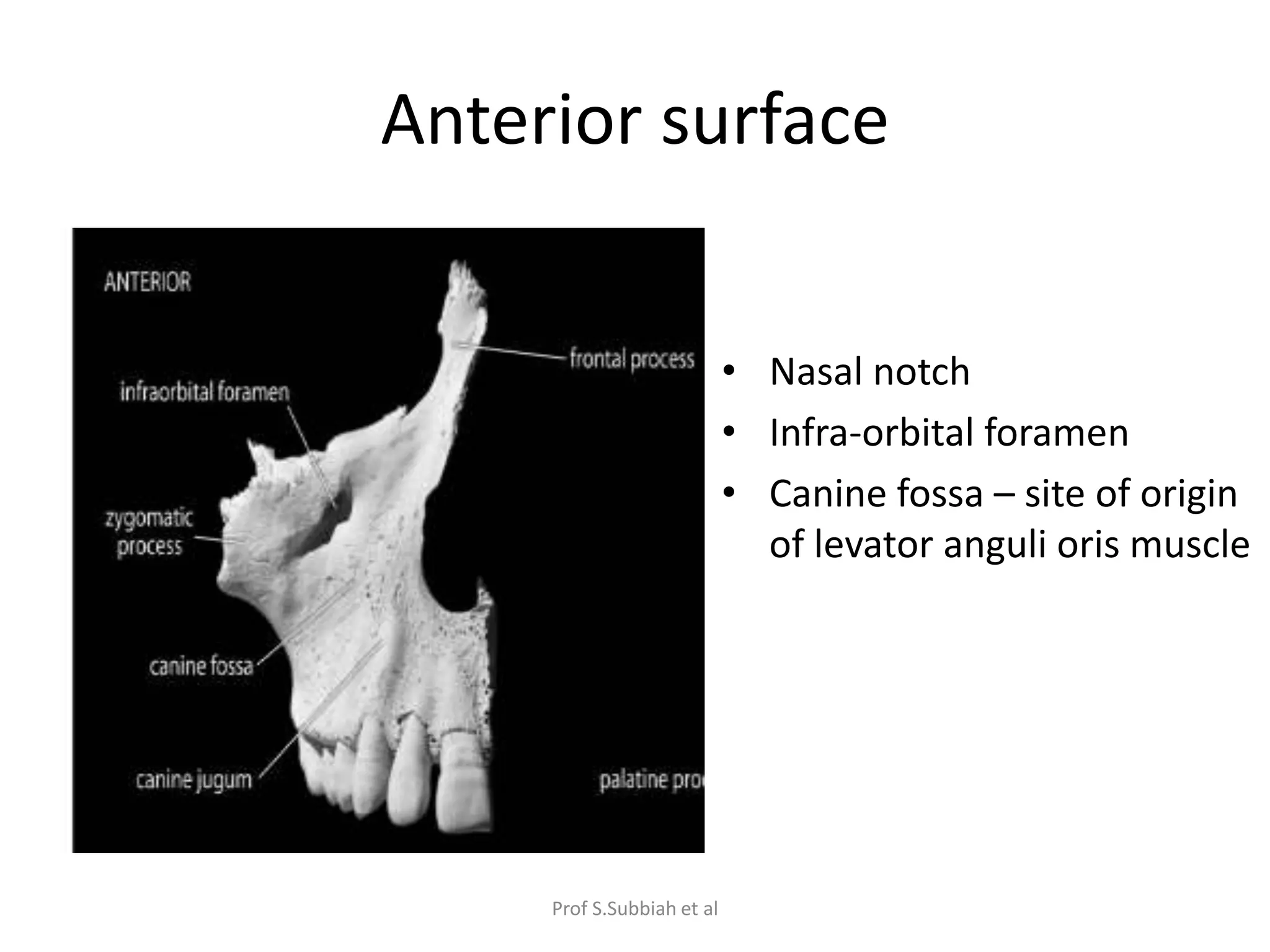
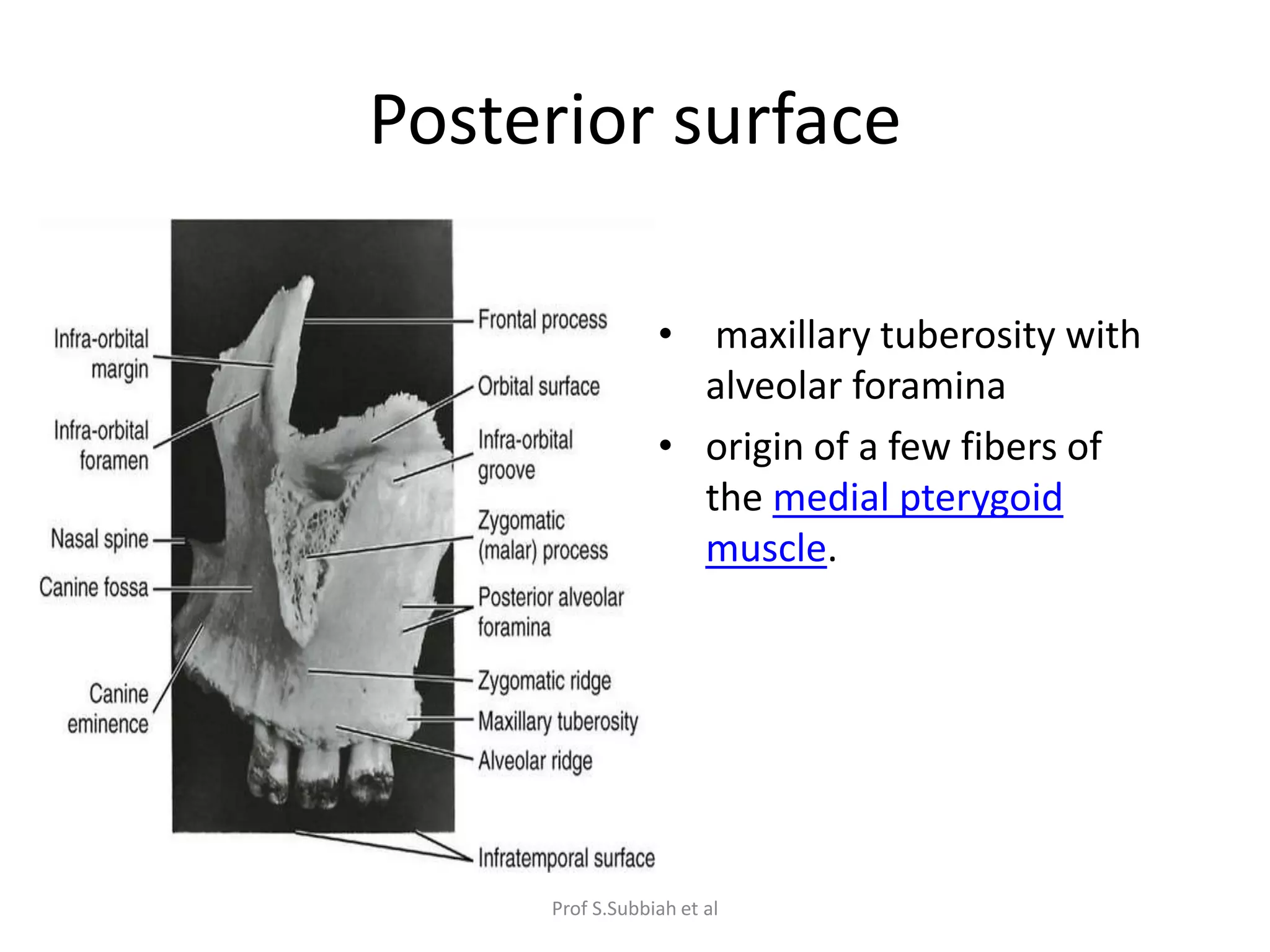
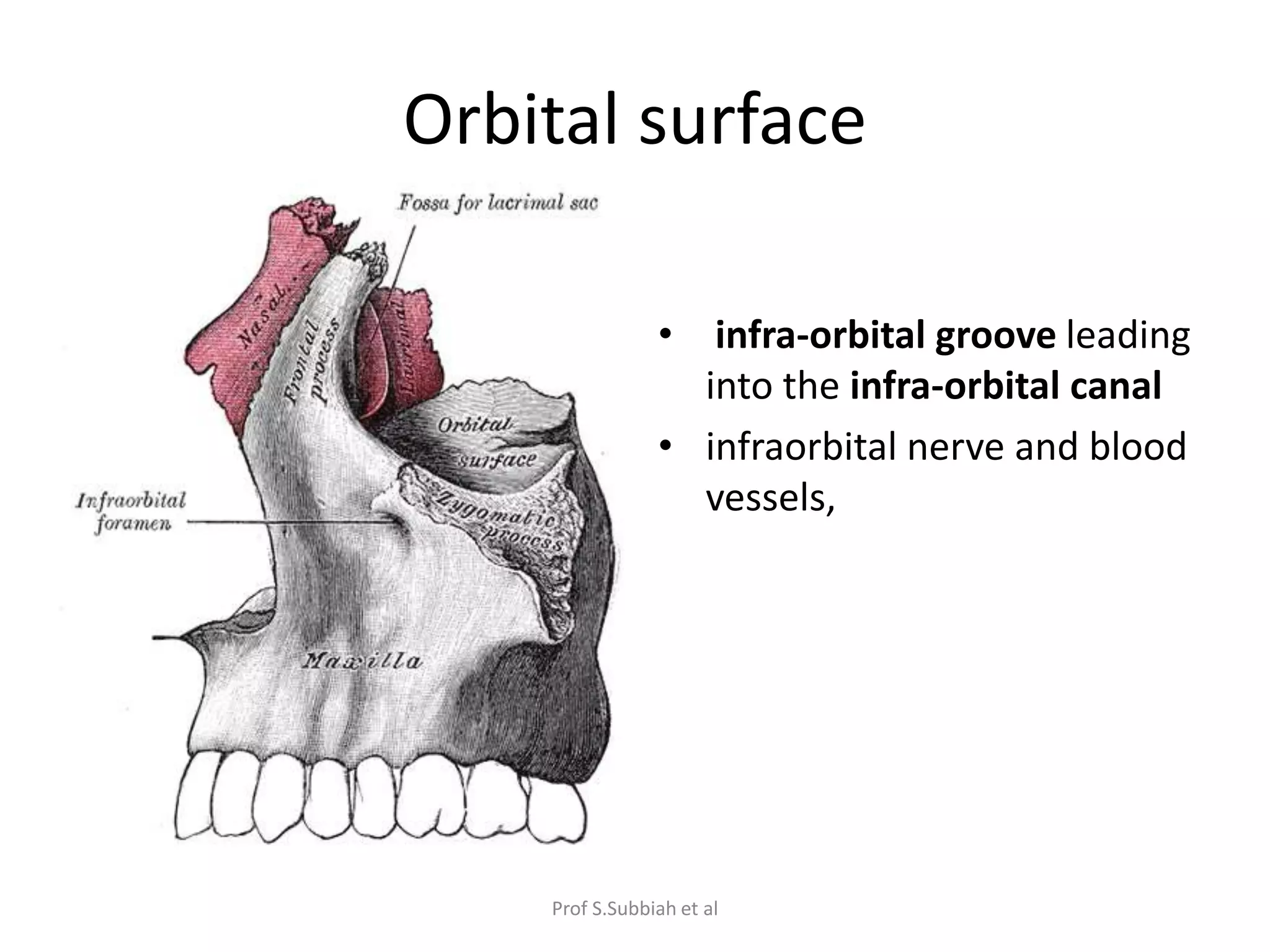
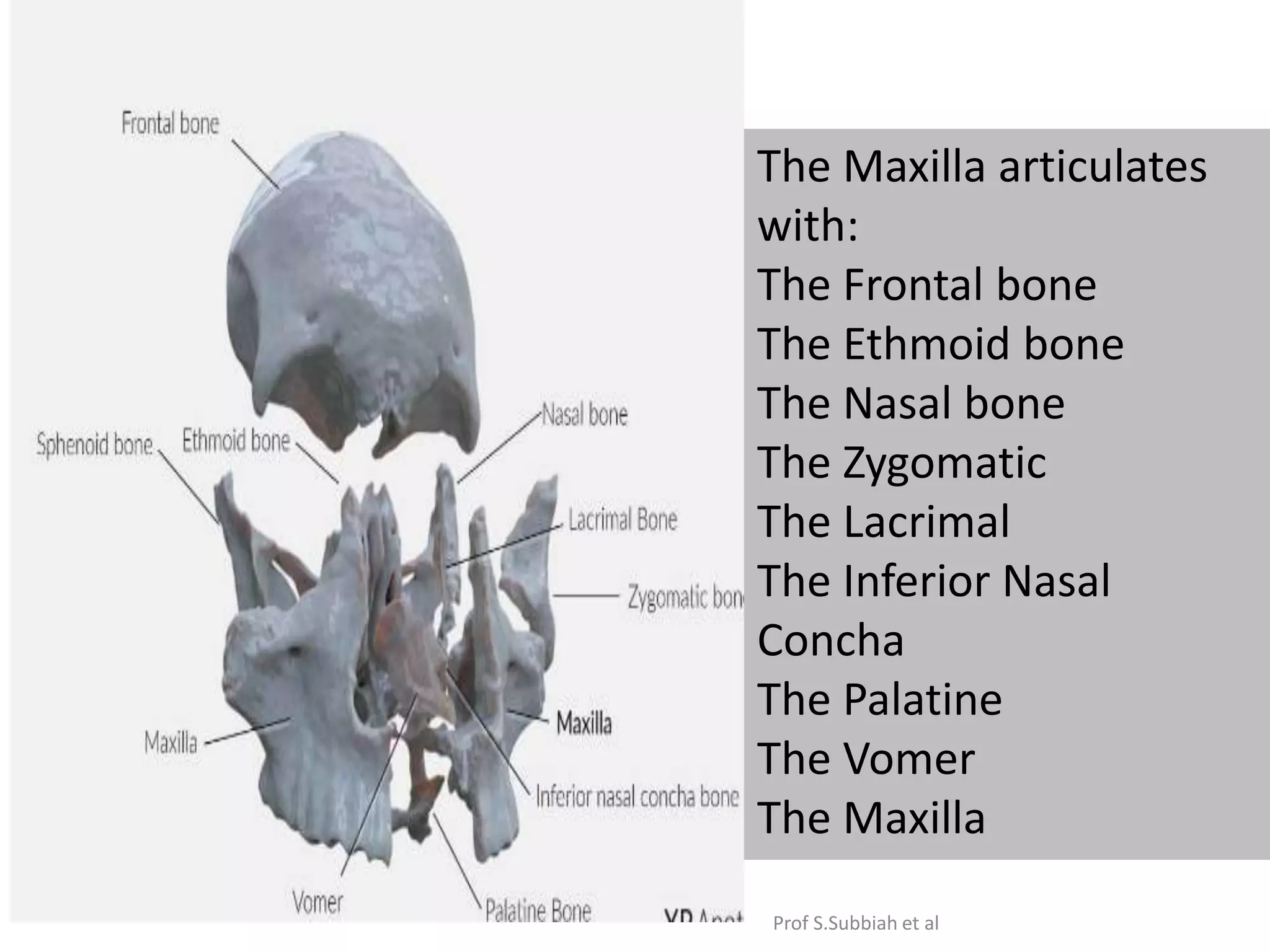
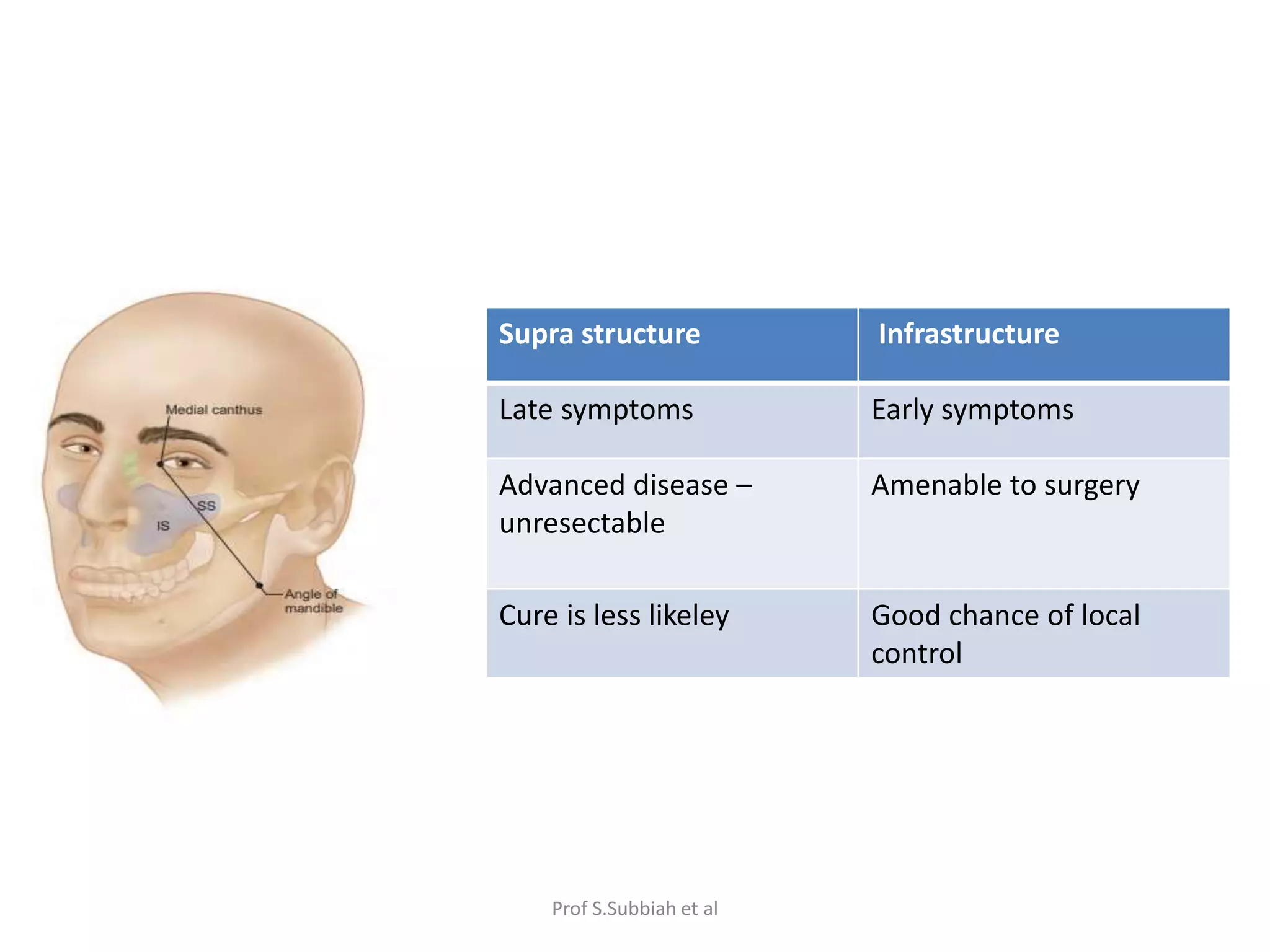
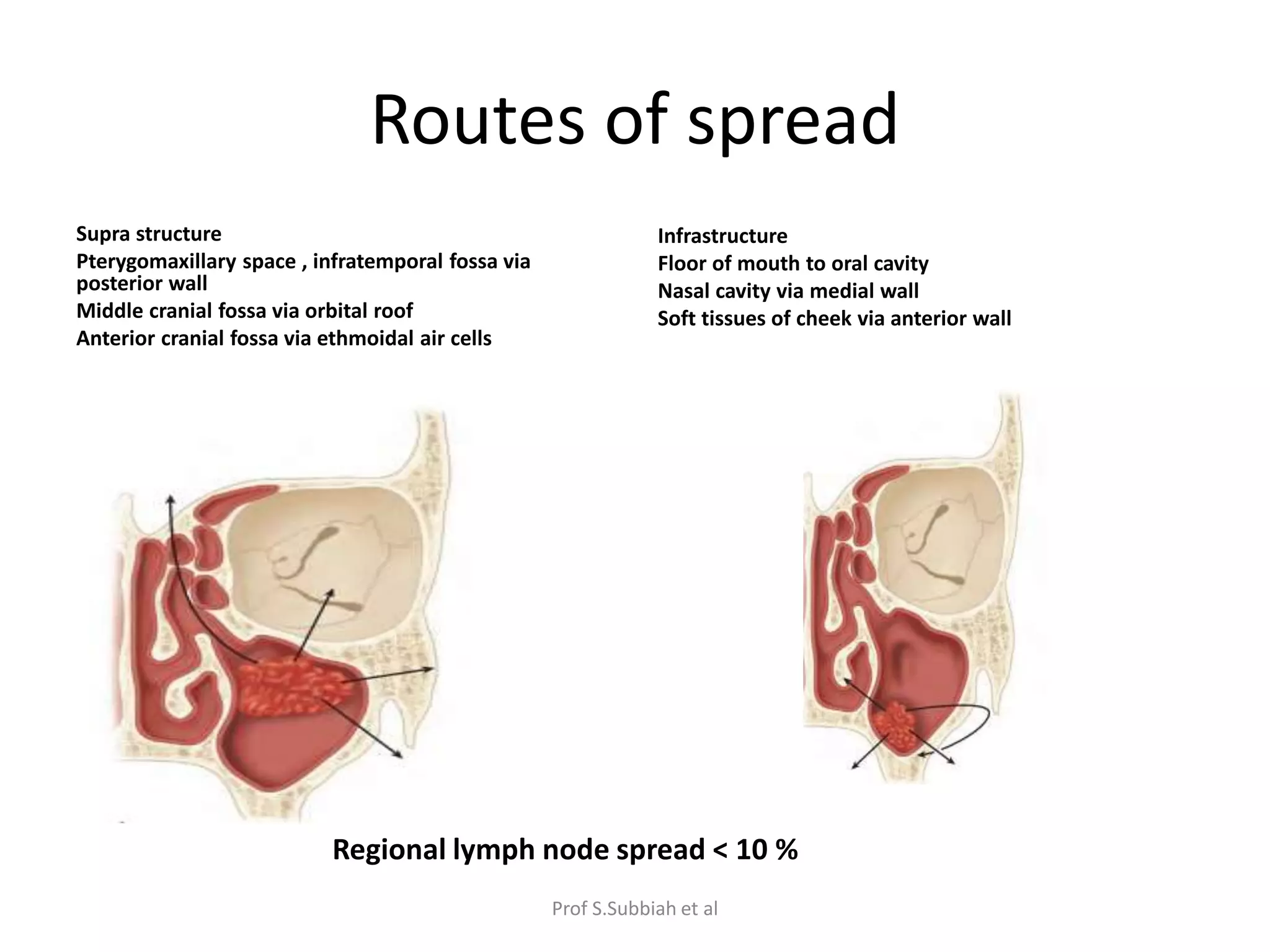
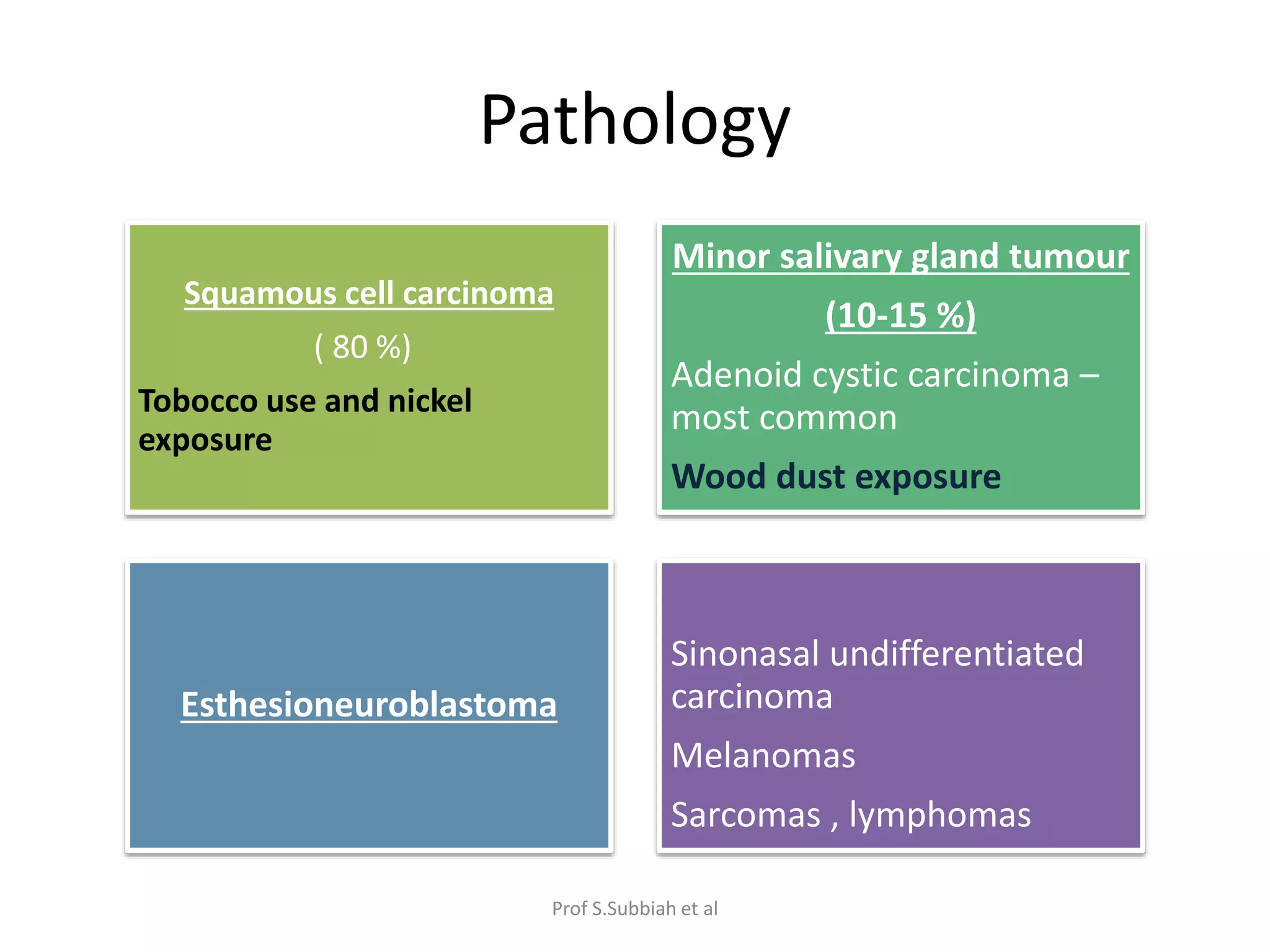
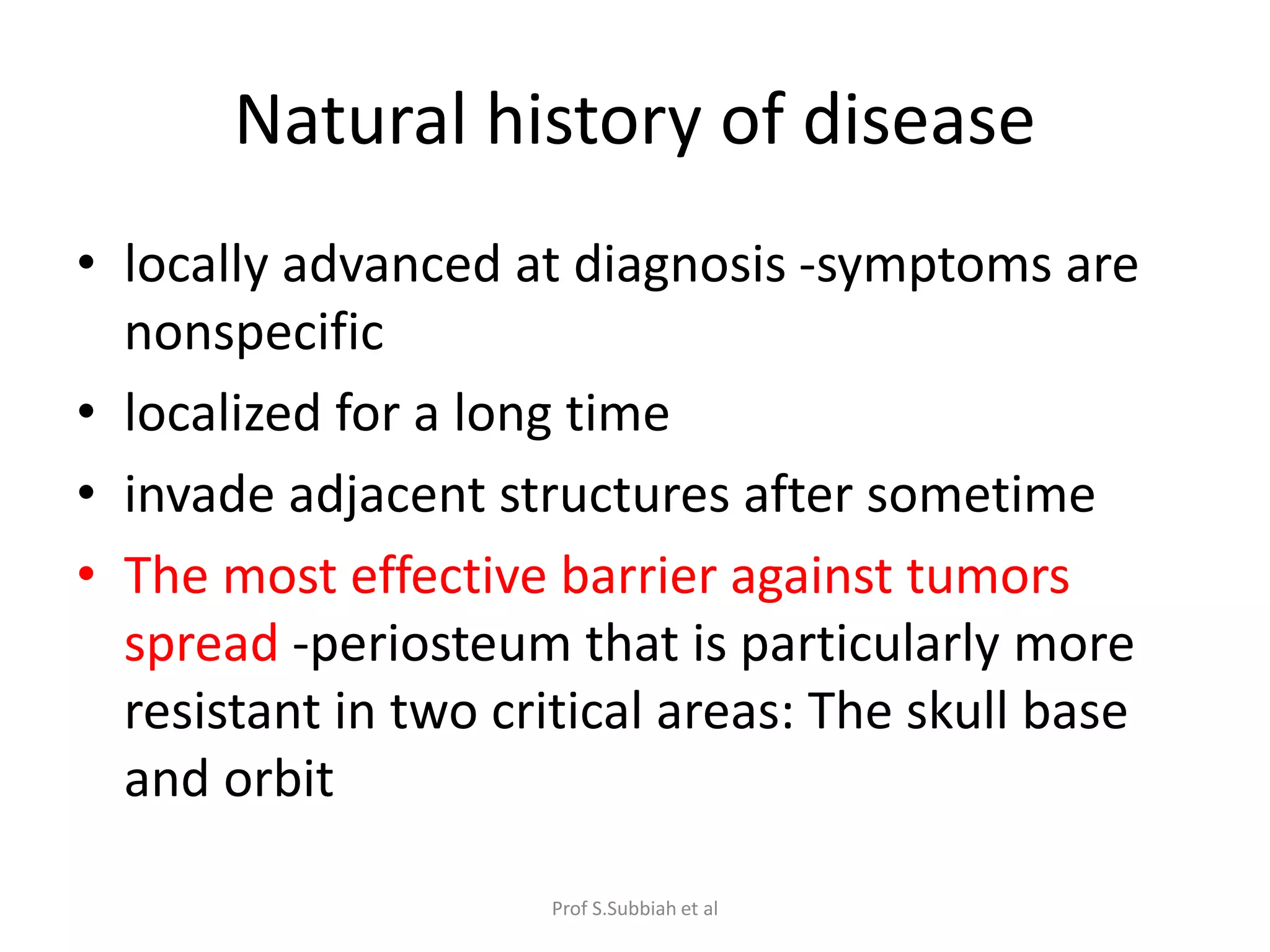
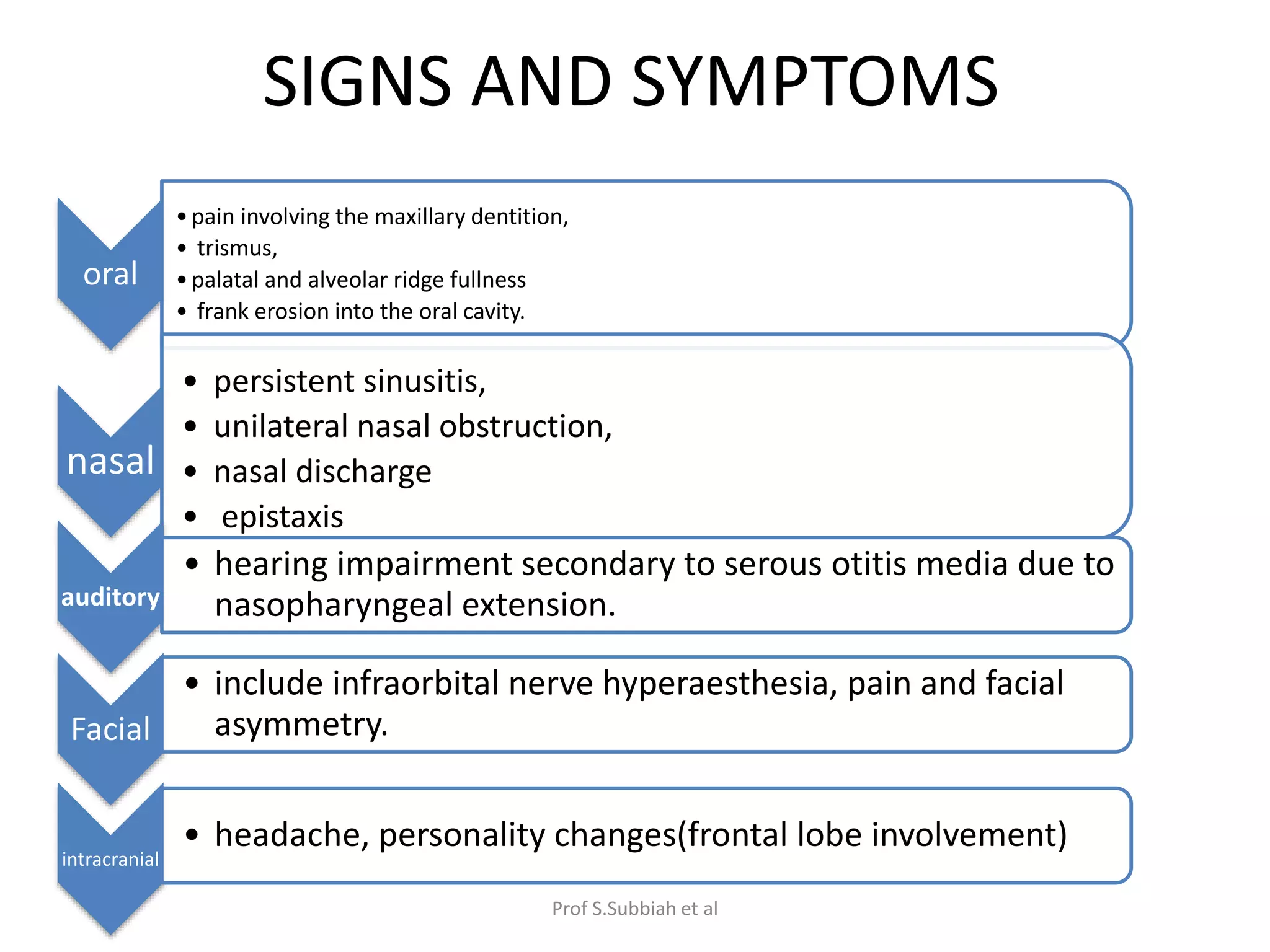
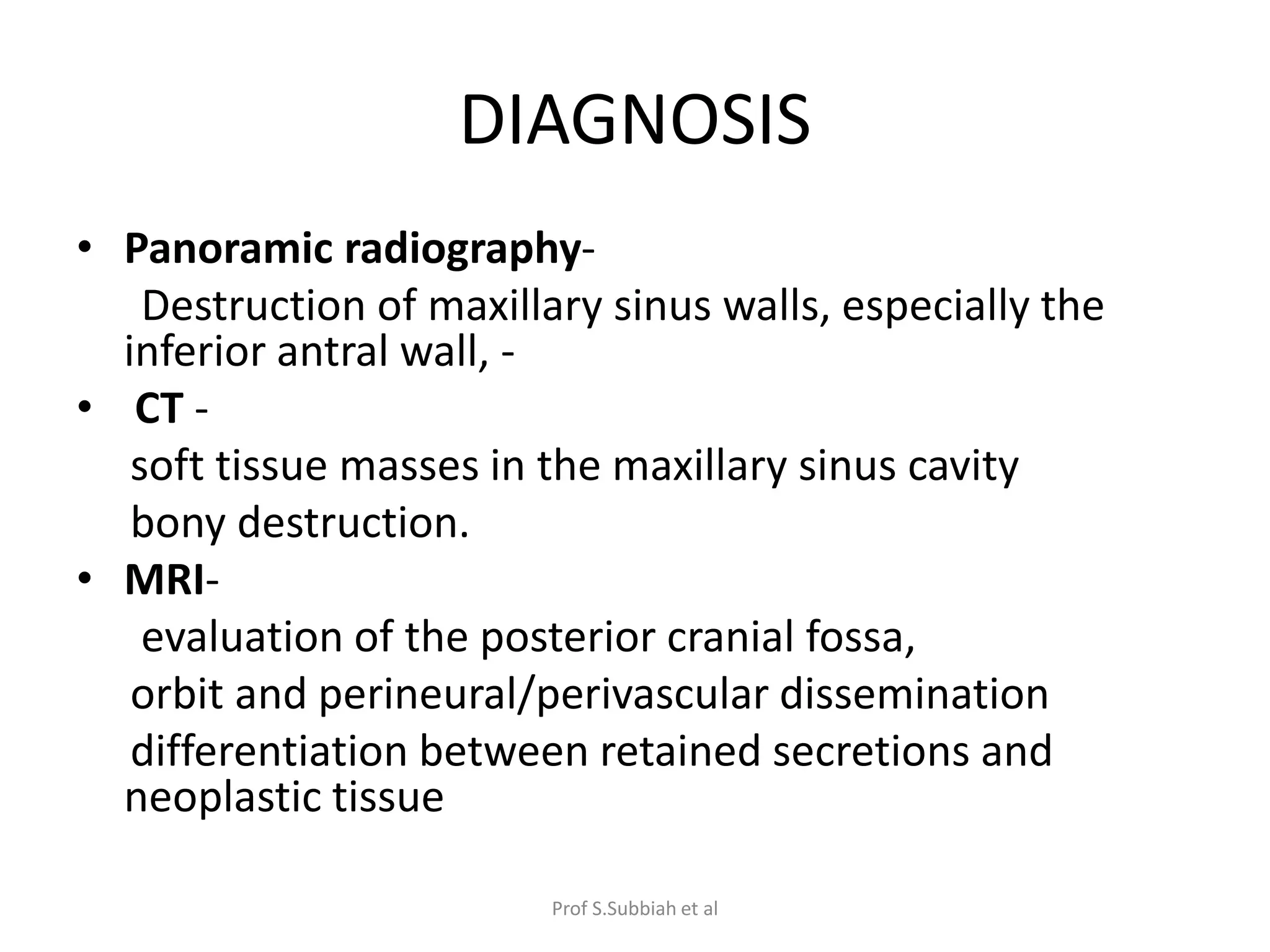
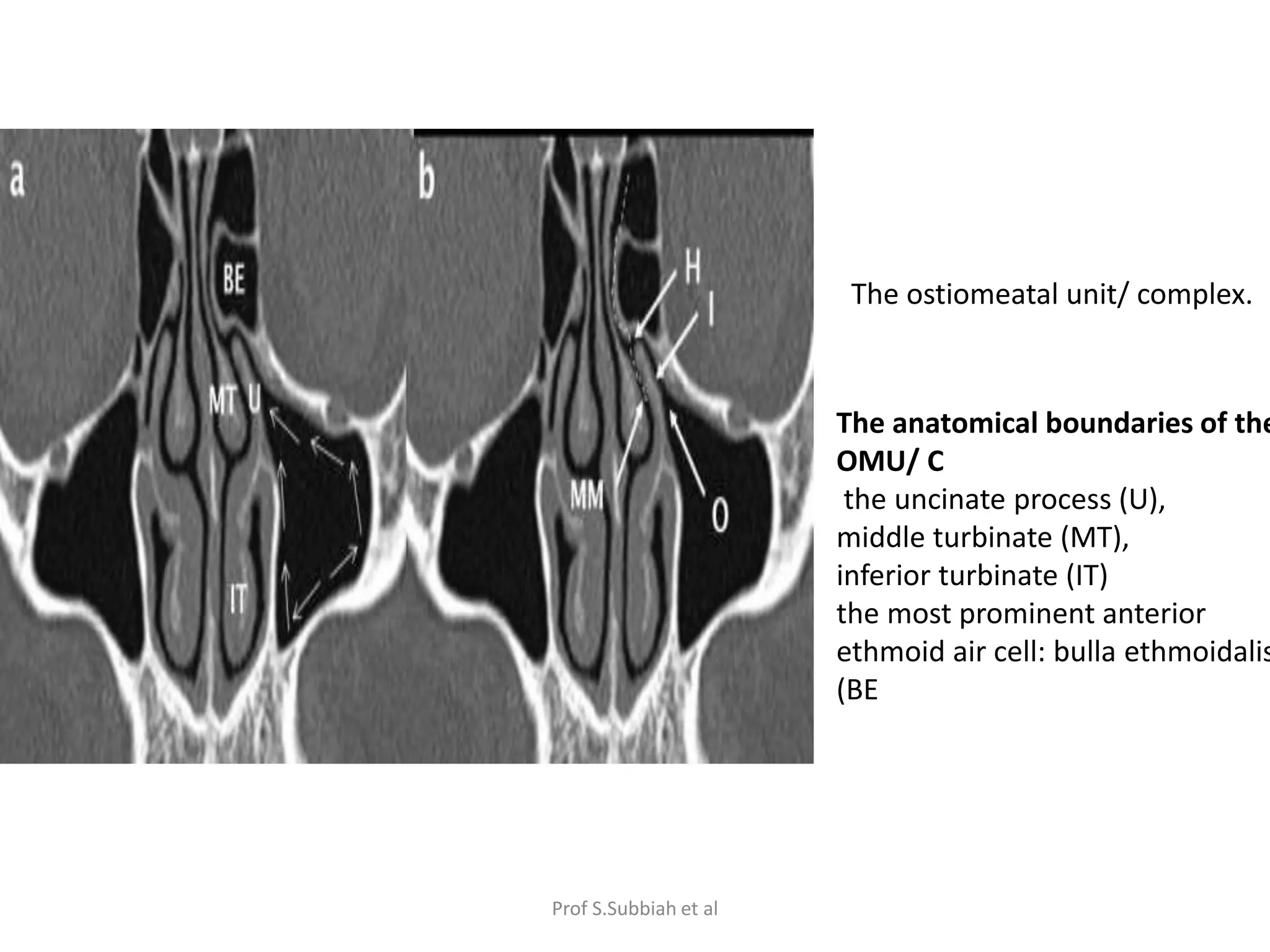
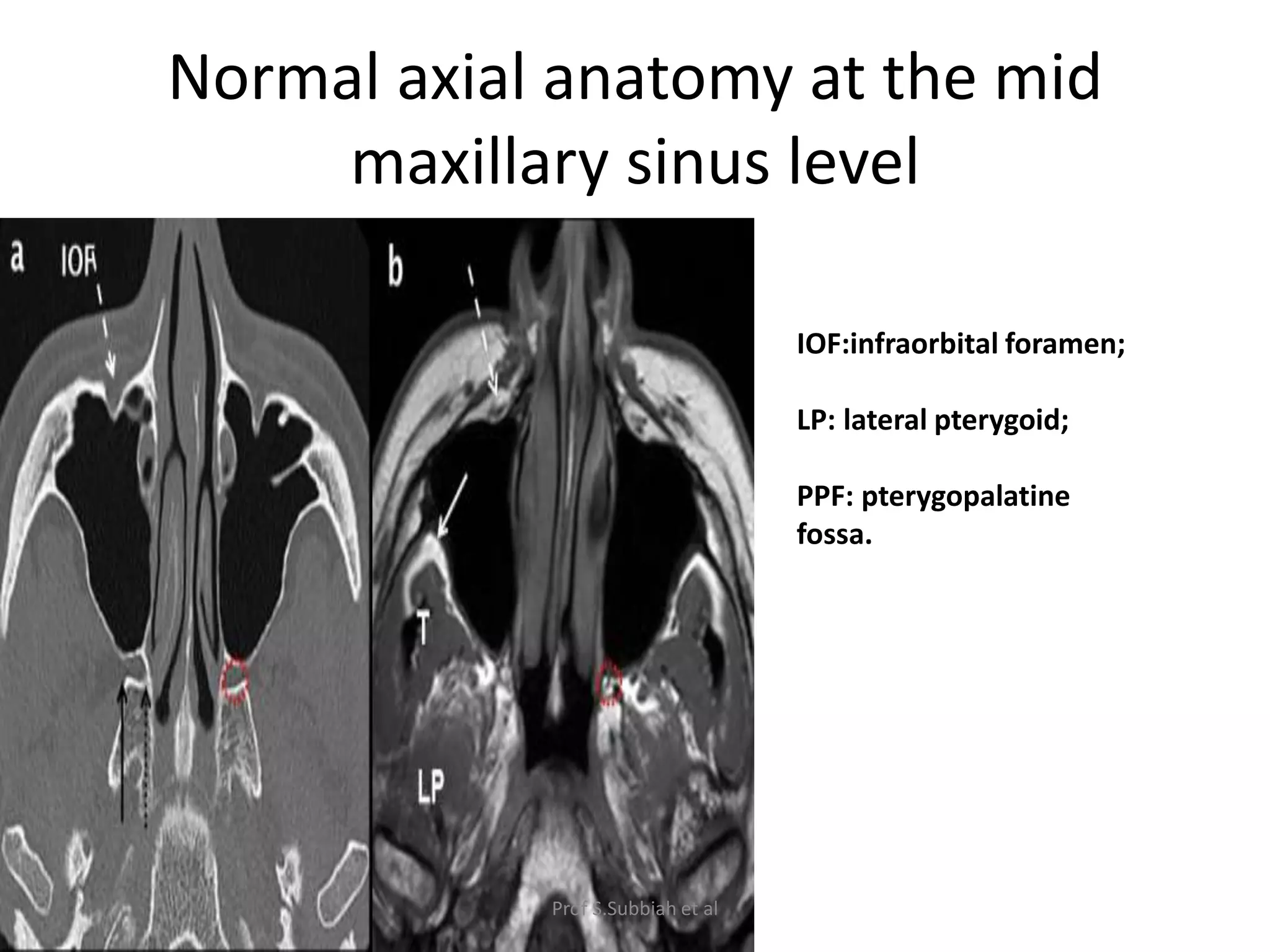
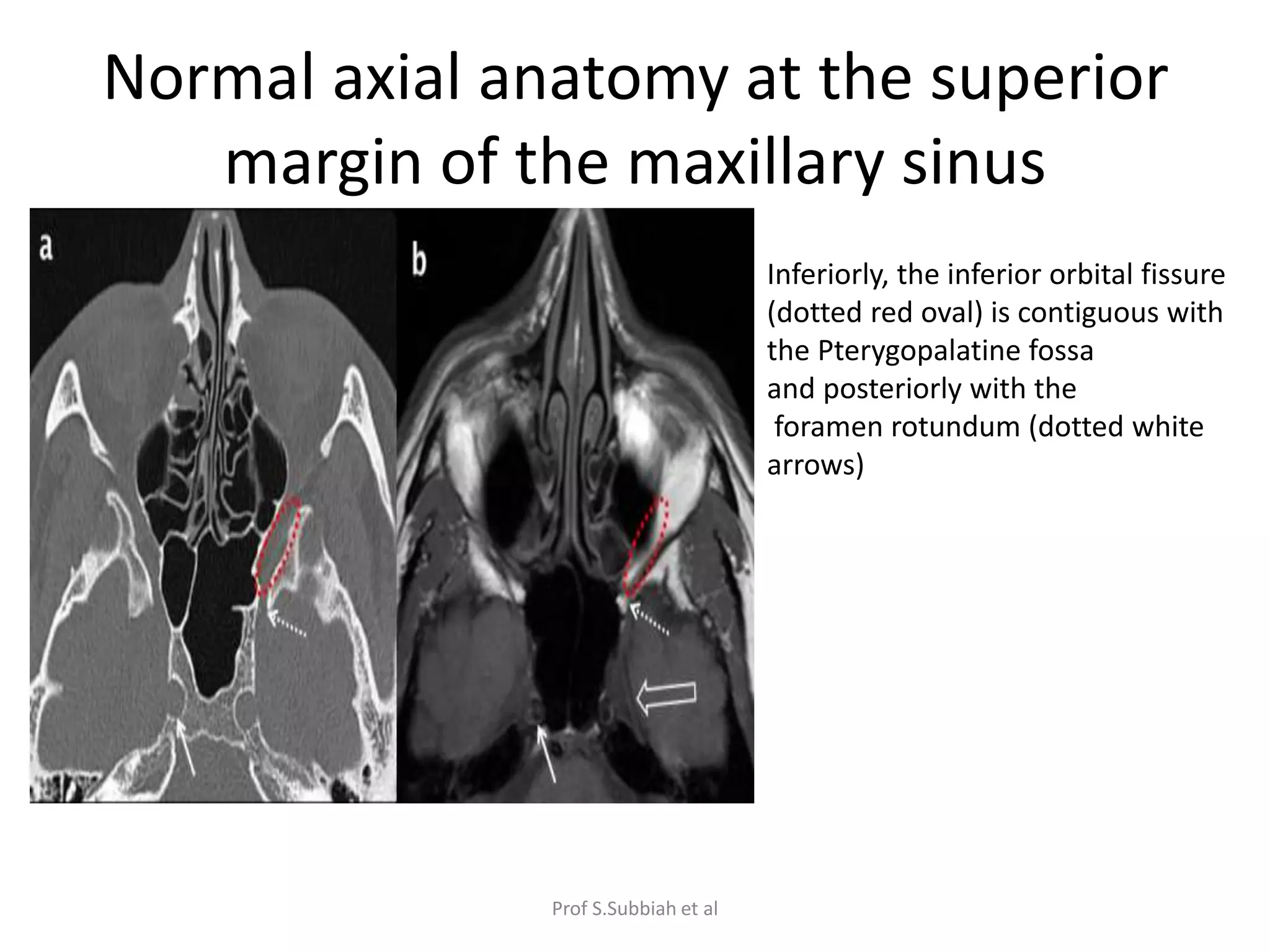
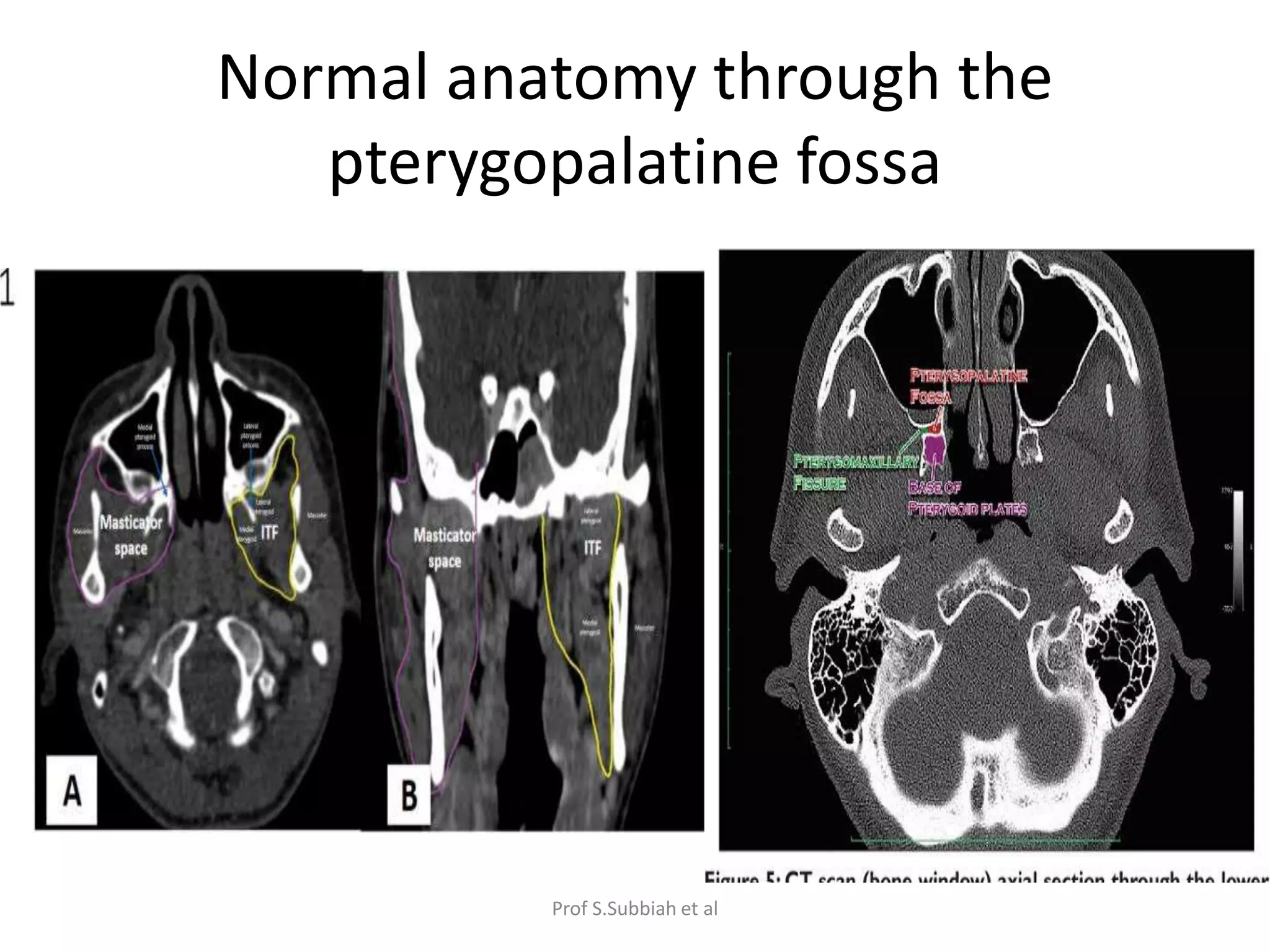
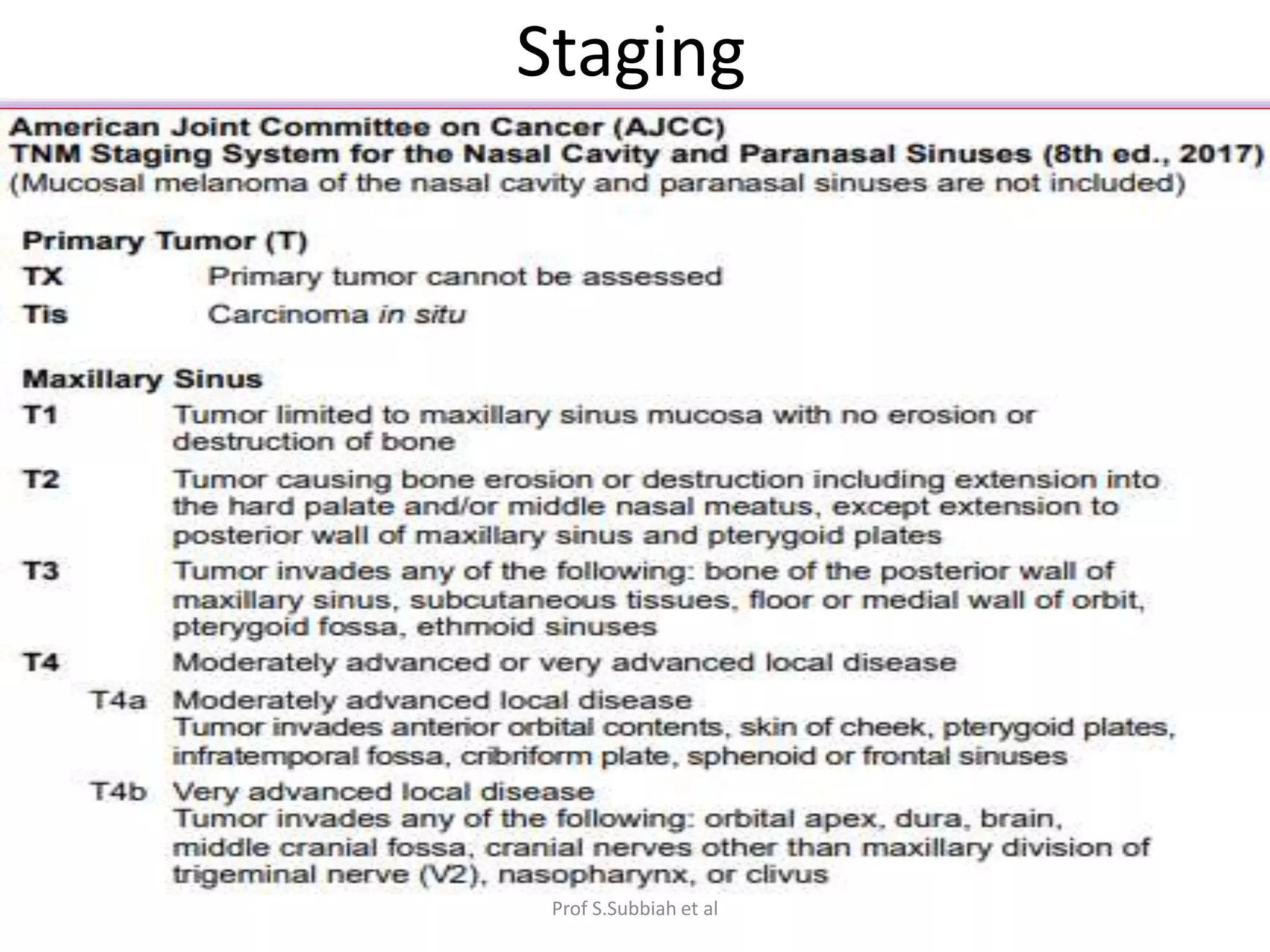
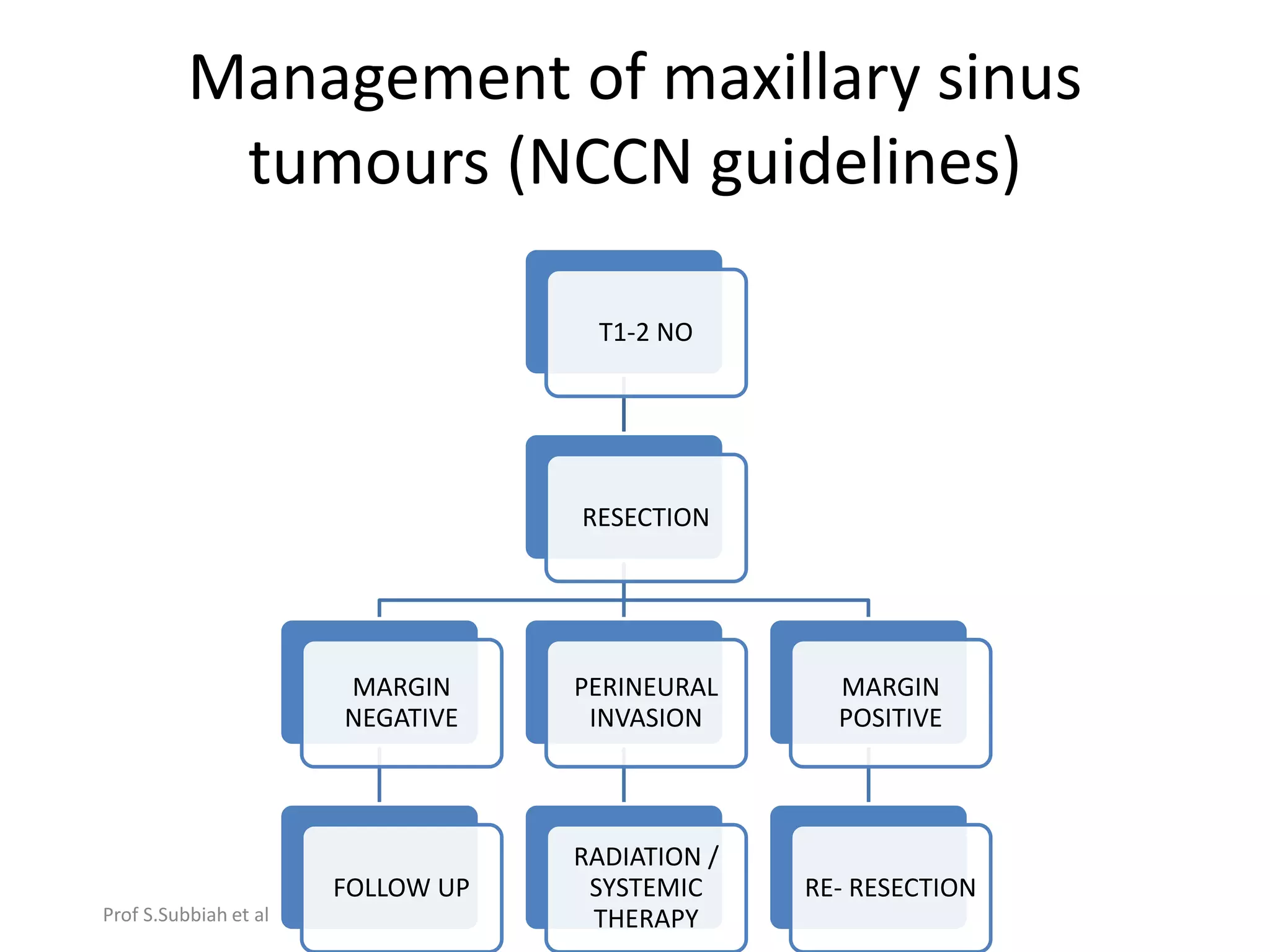
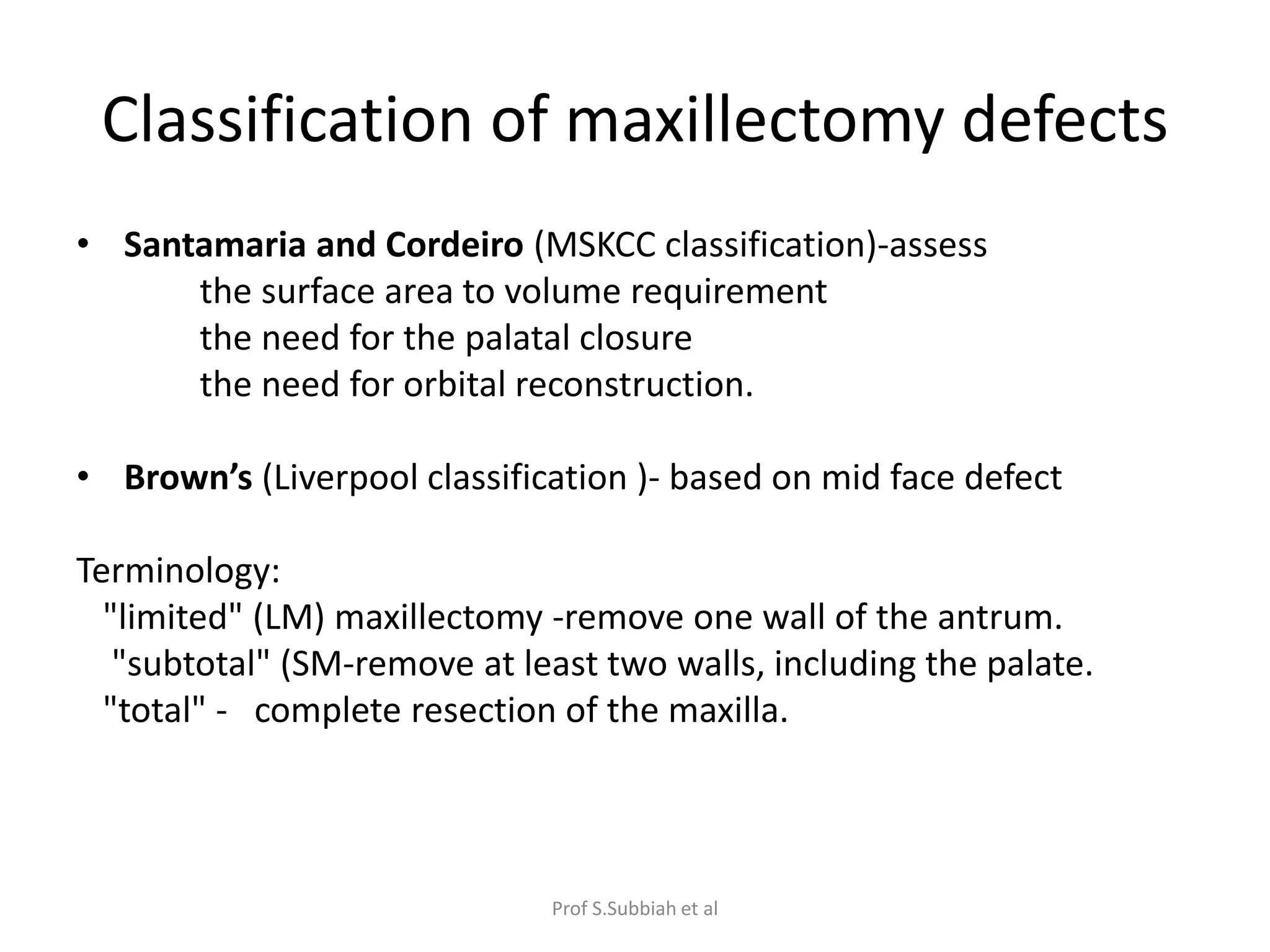
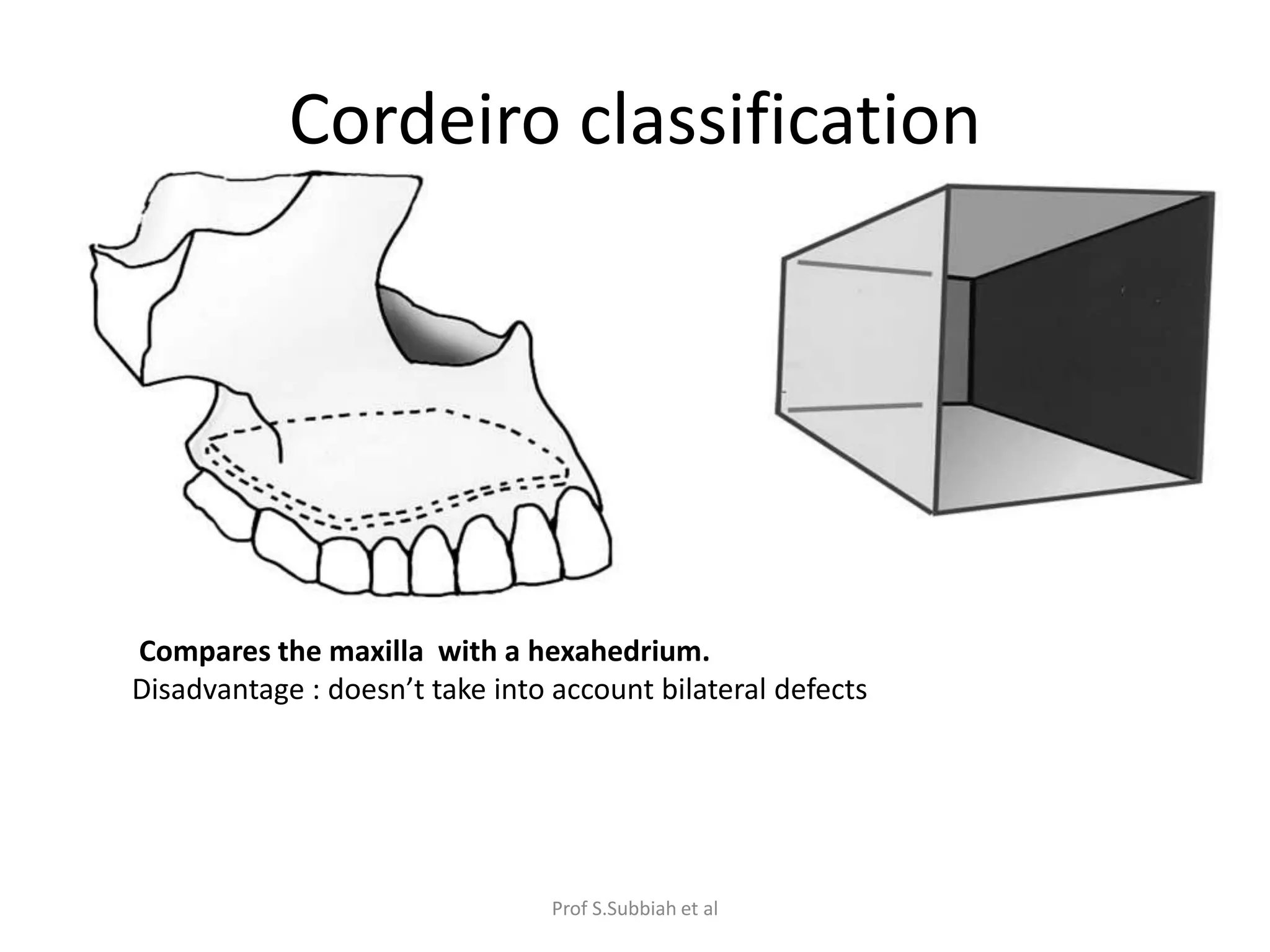
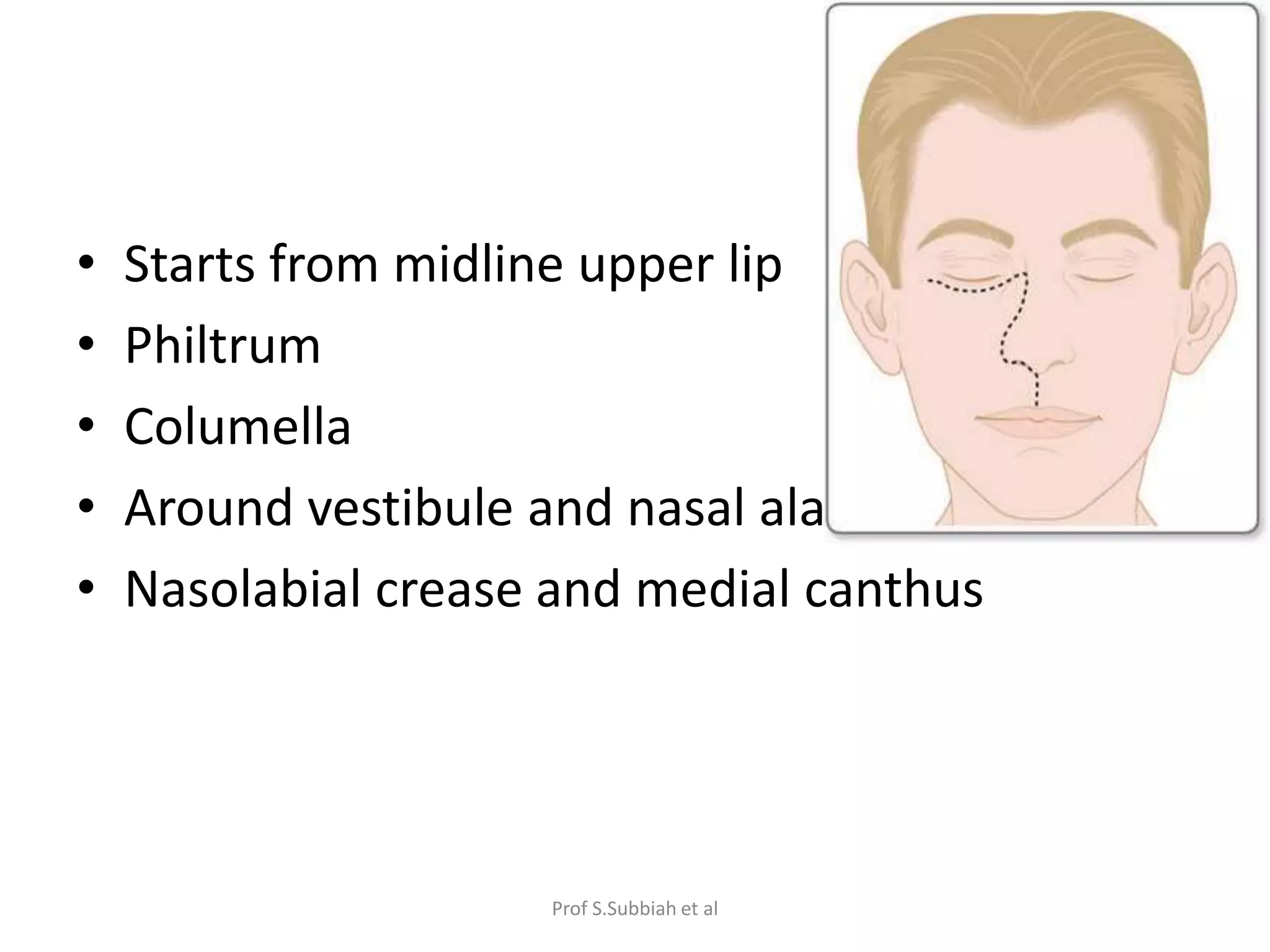
Carcinoma of the maxillary sinus is rare, constituting 3-5% of head and neck cancers. The maxillary sinus is the most common site. Anatomy of the maxilla includes processes, surfaces, and articulations with other bones. Maxillary sinus boundaries include the roof, medial wall, floor, and buttresses. Ohngren's line divides lesions into suprastructure and infrastructure types. Spread can occur via routes like the pterygomaxillary space. Risk factors include wood dust and HPV. Pathology is usually squamous cell carcinoma. Symptoms include oral, nasal, auditory, and facial issues. Diagnosis involves imaging like CT and MRI. Management involves surgery with or without radiation depending on