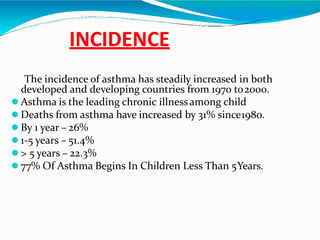
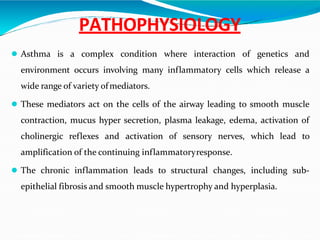
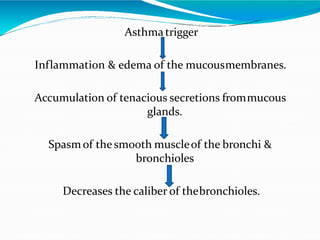
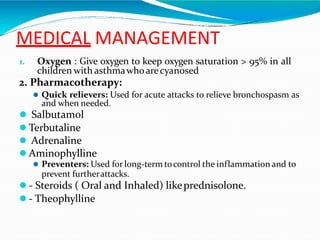
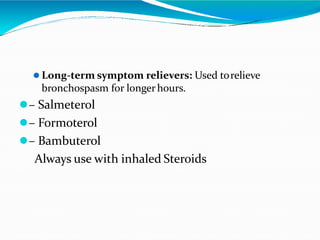
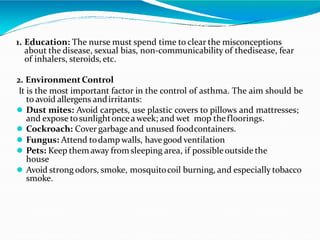
Asthma is a chronic lung disease characterized by airway inflammation, obstruction, and hyper-reactivity, with increasing incidence rates, especially among children. Its triggers include environmental allergens, infections, and certain foods, leading to clinical manifestations like dyspnea, wheezing, and cough. Management involves pharmacotherapy, education, environmental control, emotional support, and regular follow-ups to minimize attacks and improve quality of life.