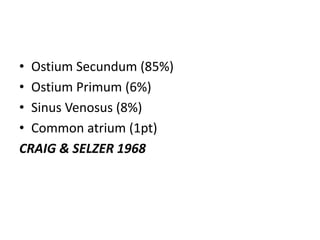
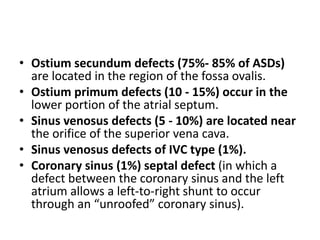
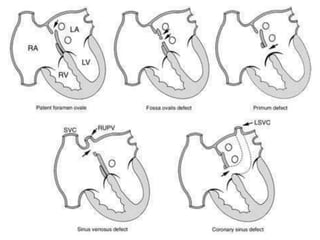
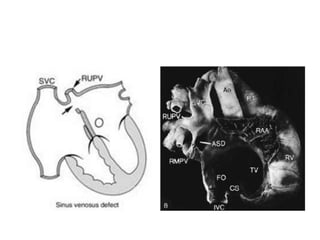
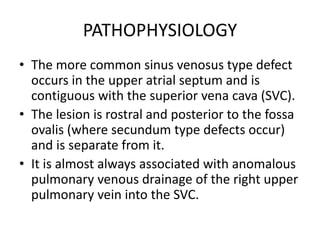
1) A sinus venosus atrial septal defect is a type of heart defect that occurs near the opening of the superior vena cava in the upper part of the atrial septum.
2) It is usually associated with anomalous drainage of the right upper pulmonary vein into the superior vena cava.
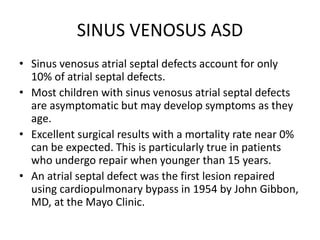
3) Surgical repair is required and involves closing the interatrial communication while also redirecting the anomalous pulmonary venous drainage into the left atrium using a patch.