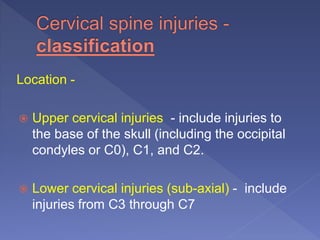
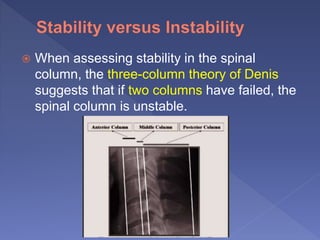
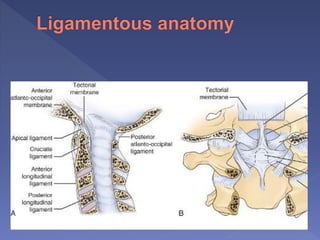
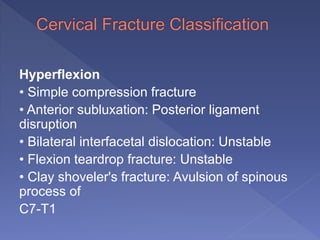
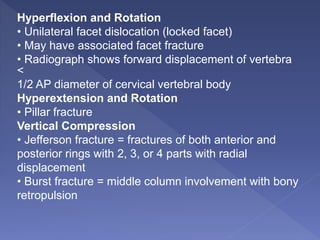
This document discusses spinal trauma, with a focus on cervical spine injuries. It provides details on:
- Epidemiology of spinal cord injuries and common causes
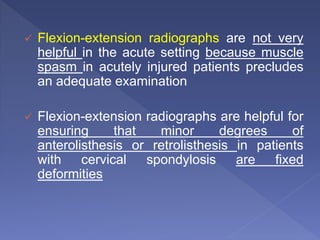
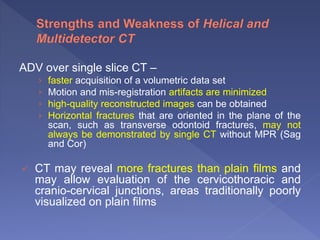
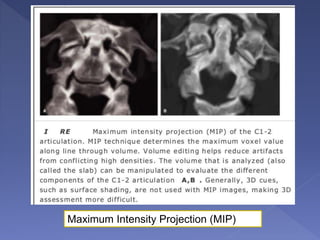
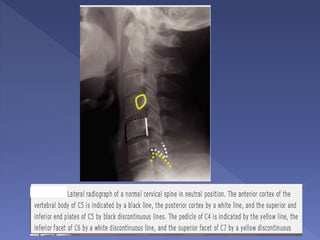
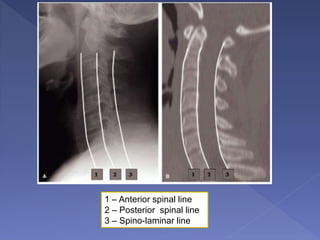
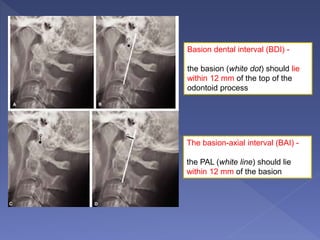
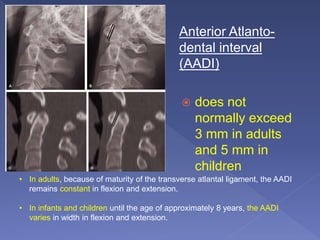
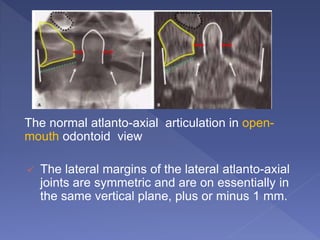
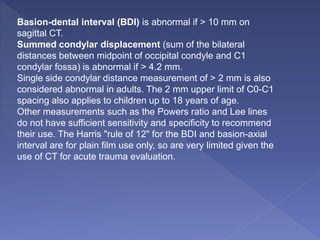
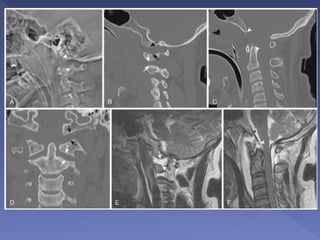
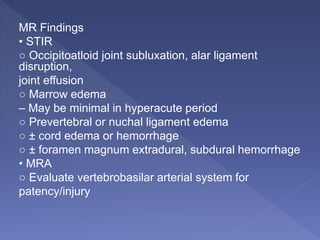
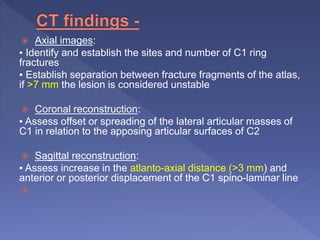
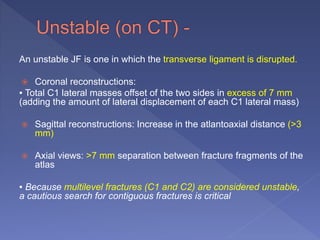
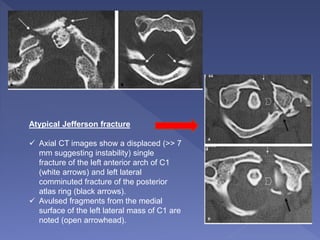
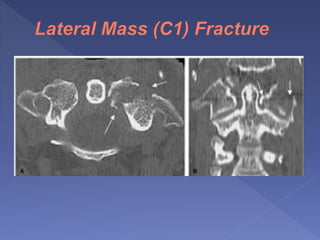
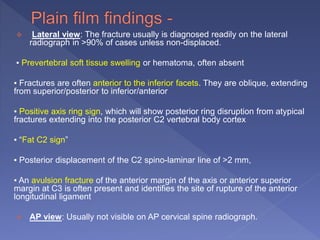
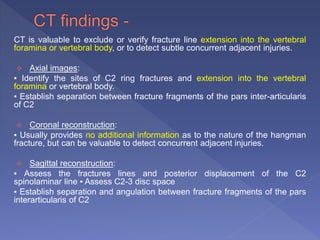
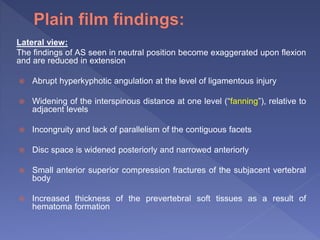
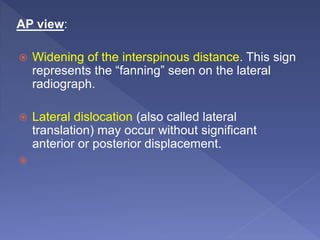
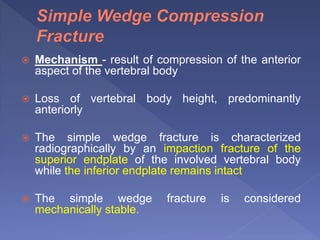
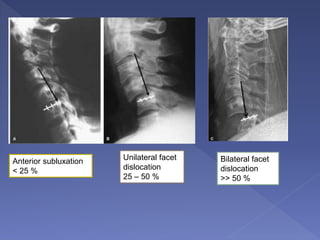
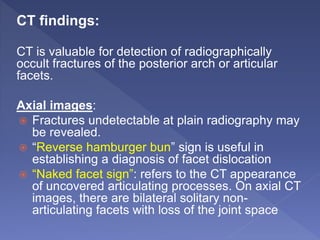
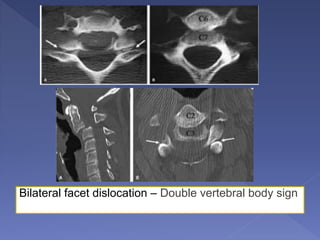
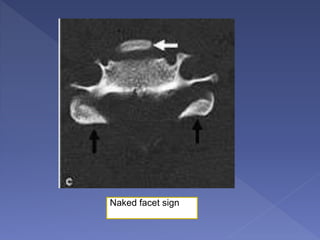
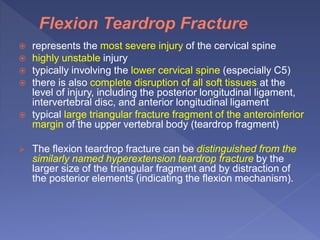
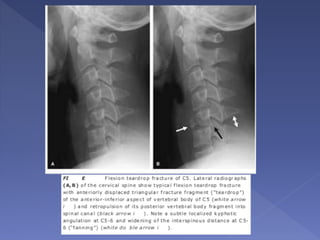
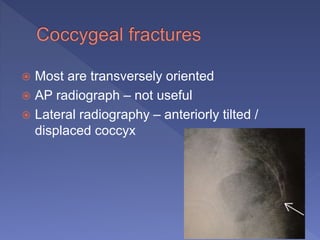
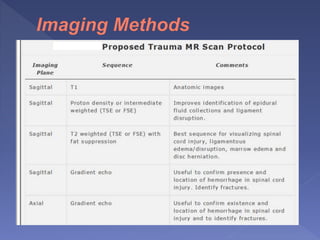
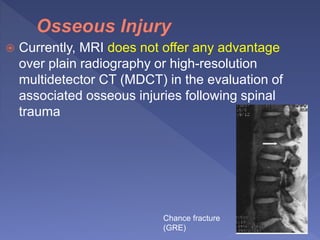
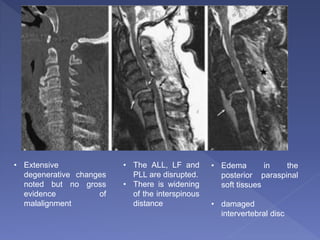
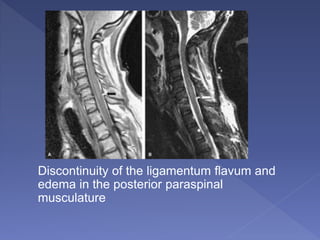
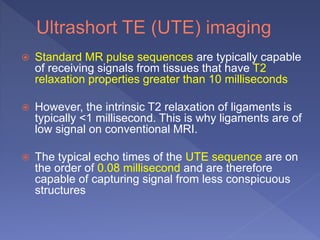
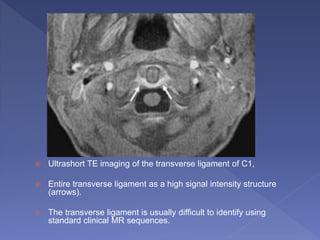
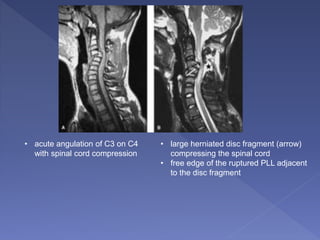
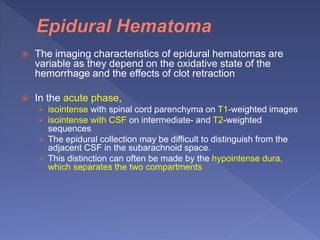
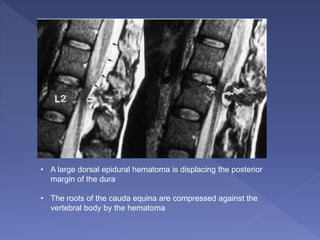
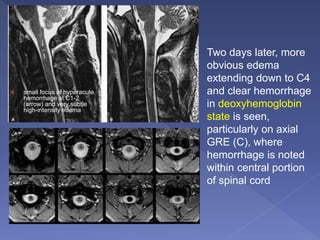
- Imaging techniques used to evaluate spinal trauma, including radiography, CT, MRI
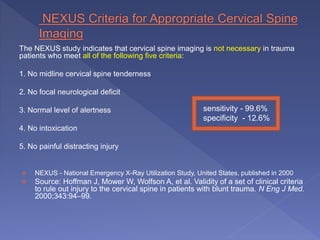
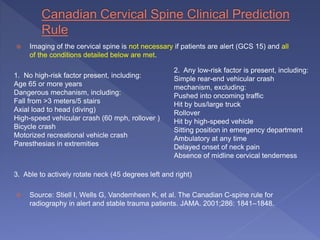
- Clinical criteria like NEXUS and Canadian C-Spine Rule that can determine if imaging is needed
- Differences in cervical spine injuries between age groups and considerations for imaging children
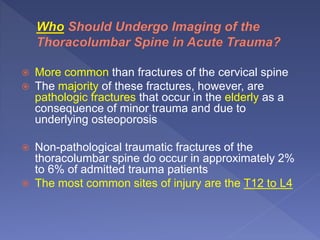
- Types of fractures more common in the elderly
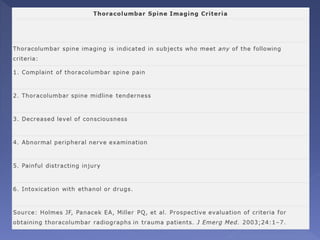
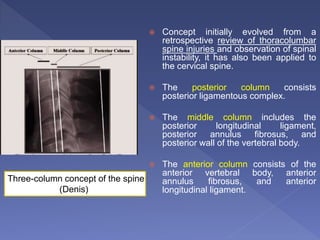
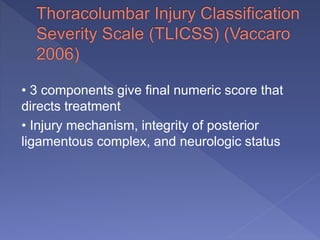
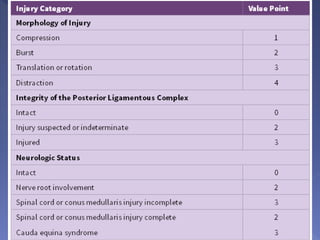
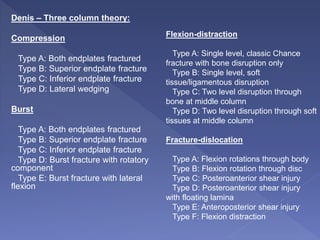
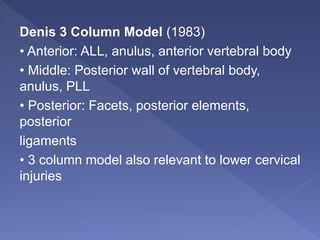
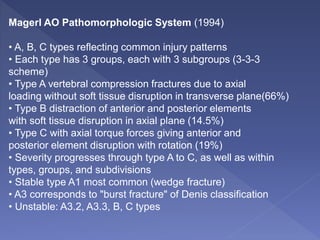
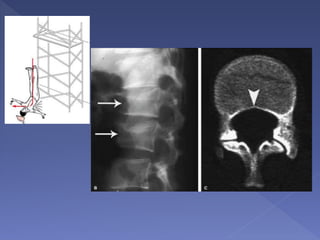
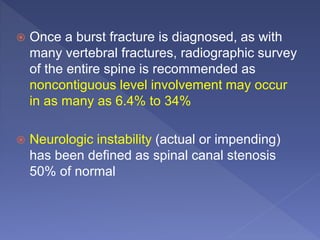
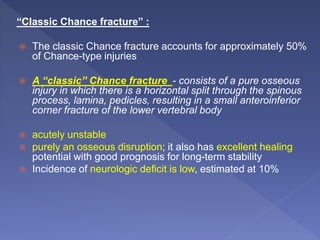
- Using CT to evaluate the thoracolumbar spine
- Advantages and limitations of various imaging modalities and techniques