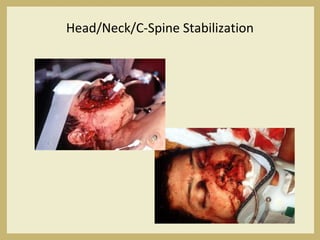
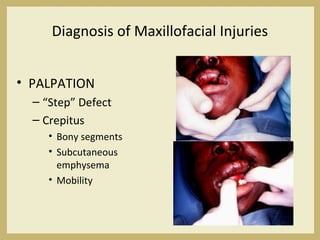
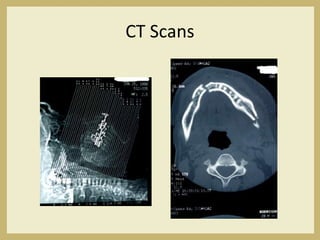
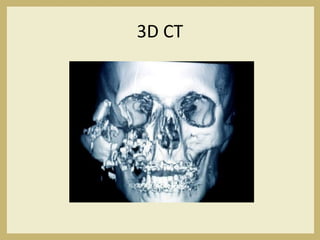
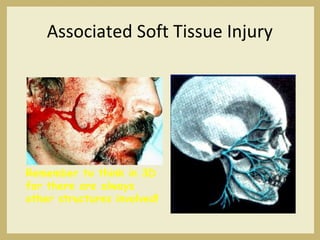
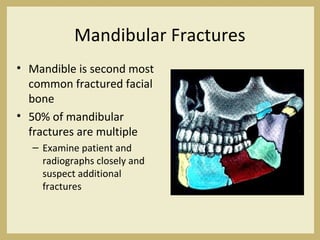
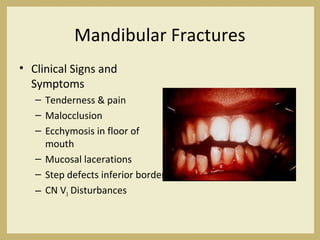
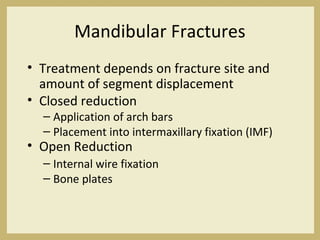
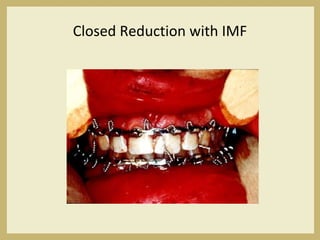
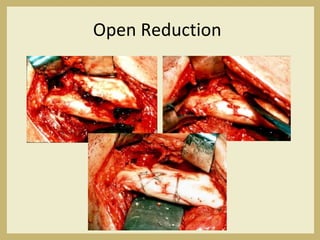
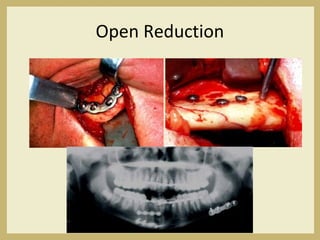
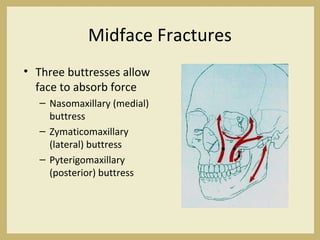
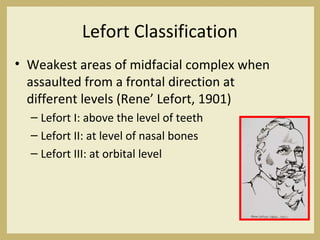
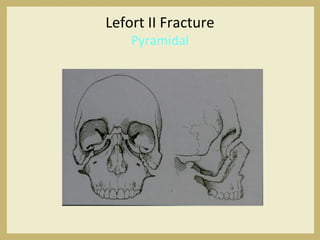
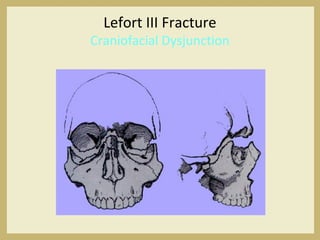
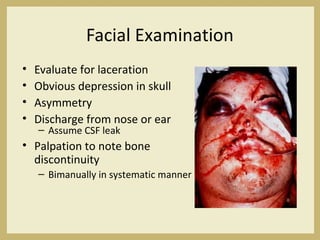
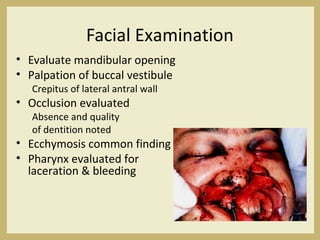
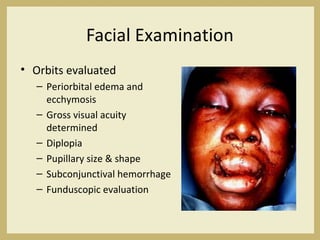
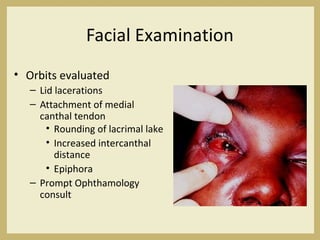
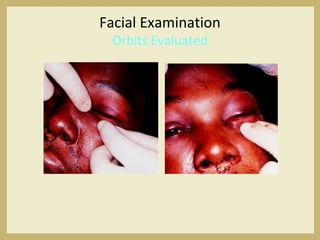
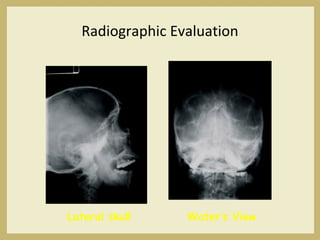
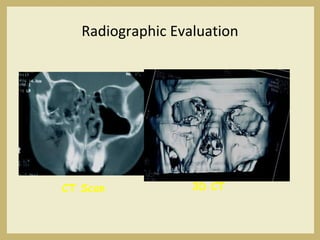
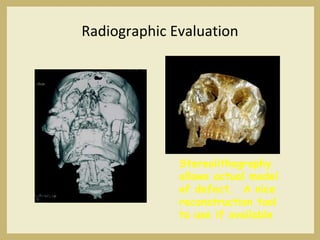
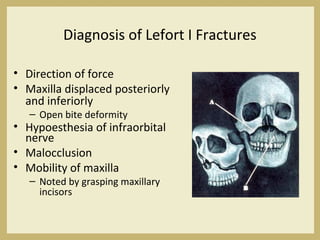
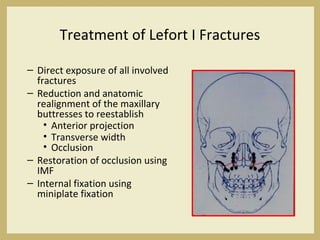
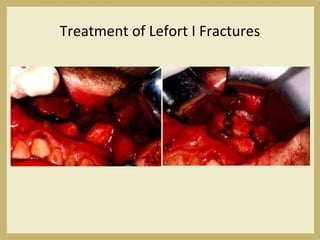
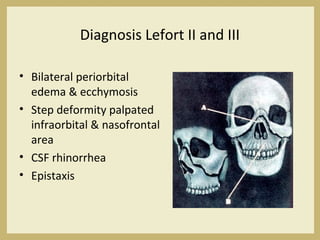
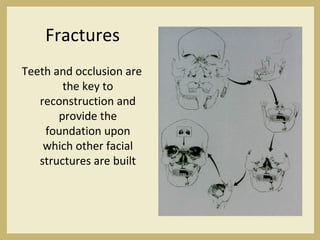
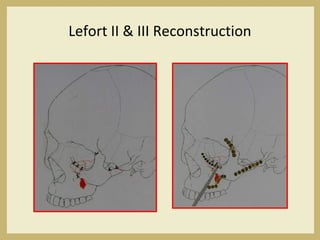
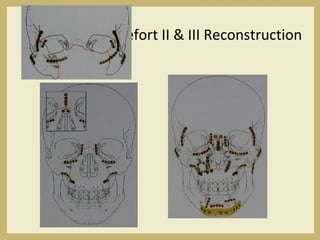
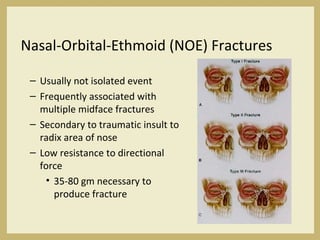
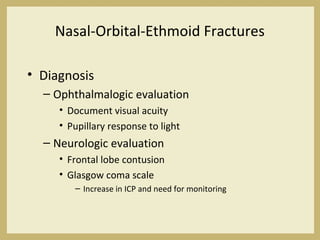
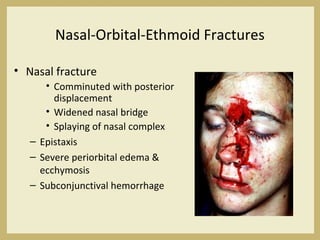
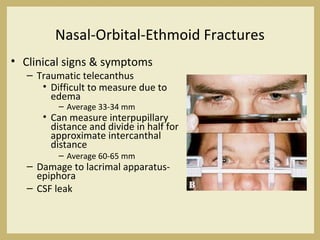
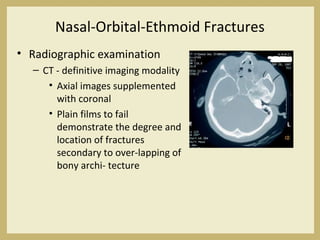
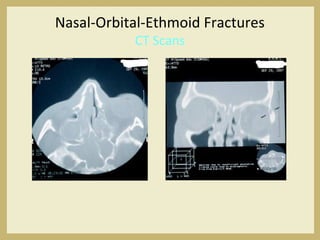
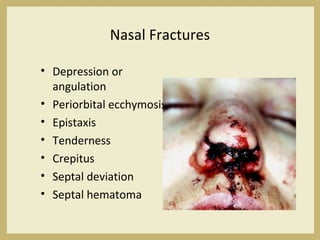
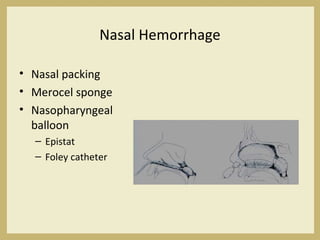
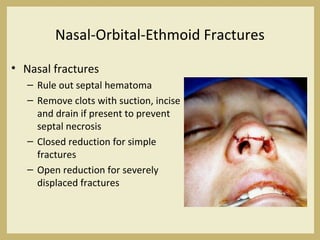
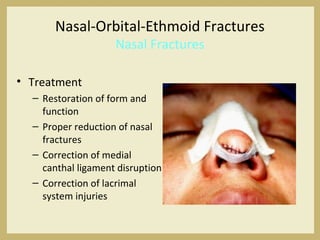
The document outlines the evaluation and management of head and neck trauma, detailing emergency, early, definitive, and secondary care phases. It emphasizes the importance of preserving the airway, controlling hemorrhage, and stabilizing cervical spine injuries, along with specific techniques for diagnosing and treating maxillofacial injuries. Additionally, it discusses various types of fractures and their management, including the Lefort classification for midface fractures and strategies for comprehensive treatment approaches involving multiple specialties.