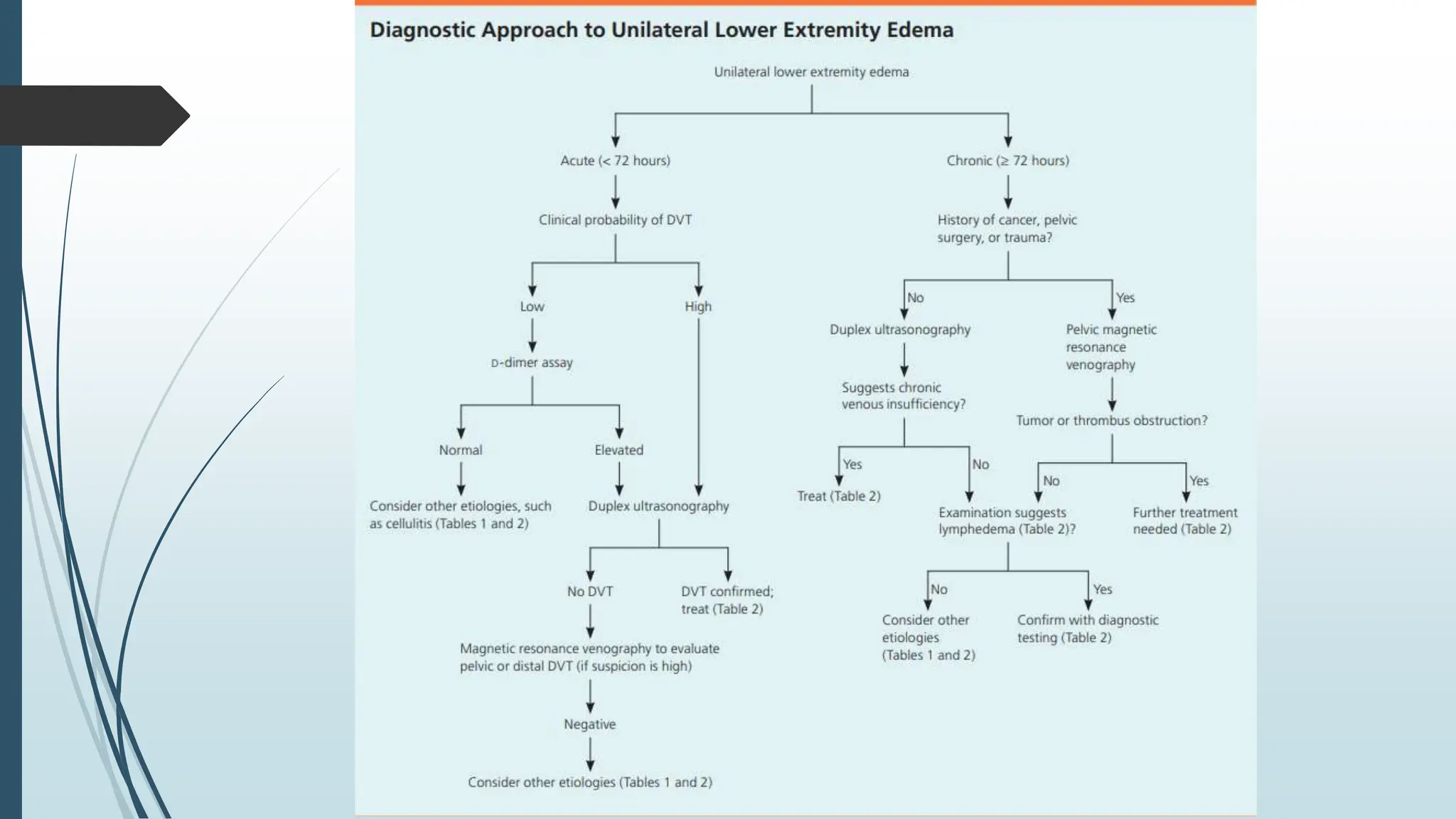
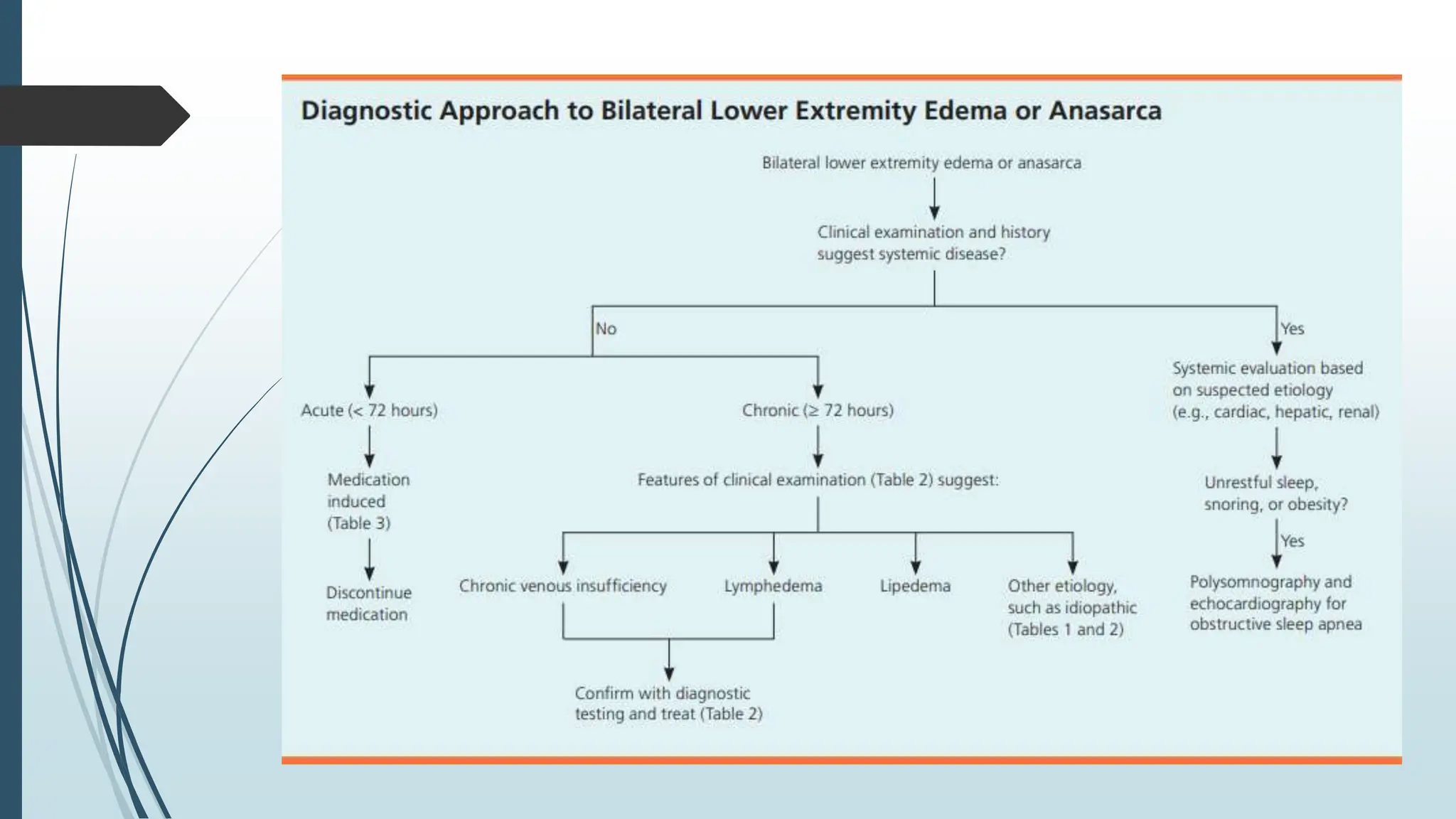
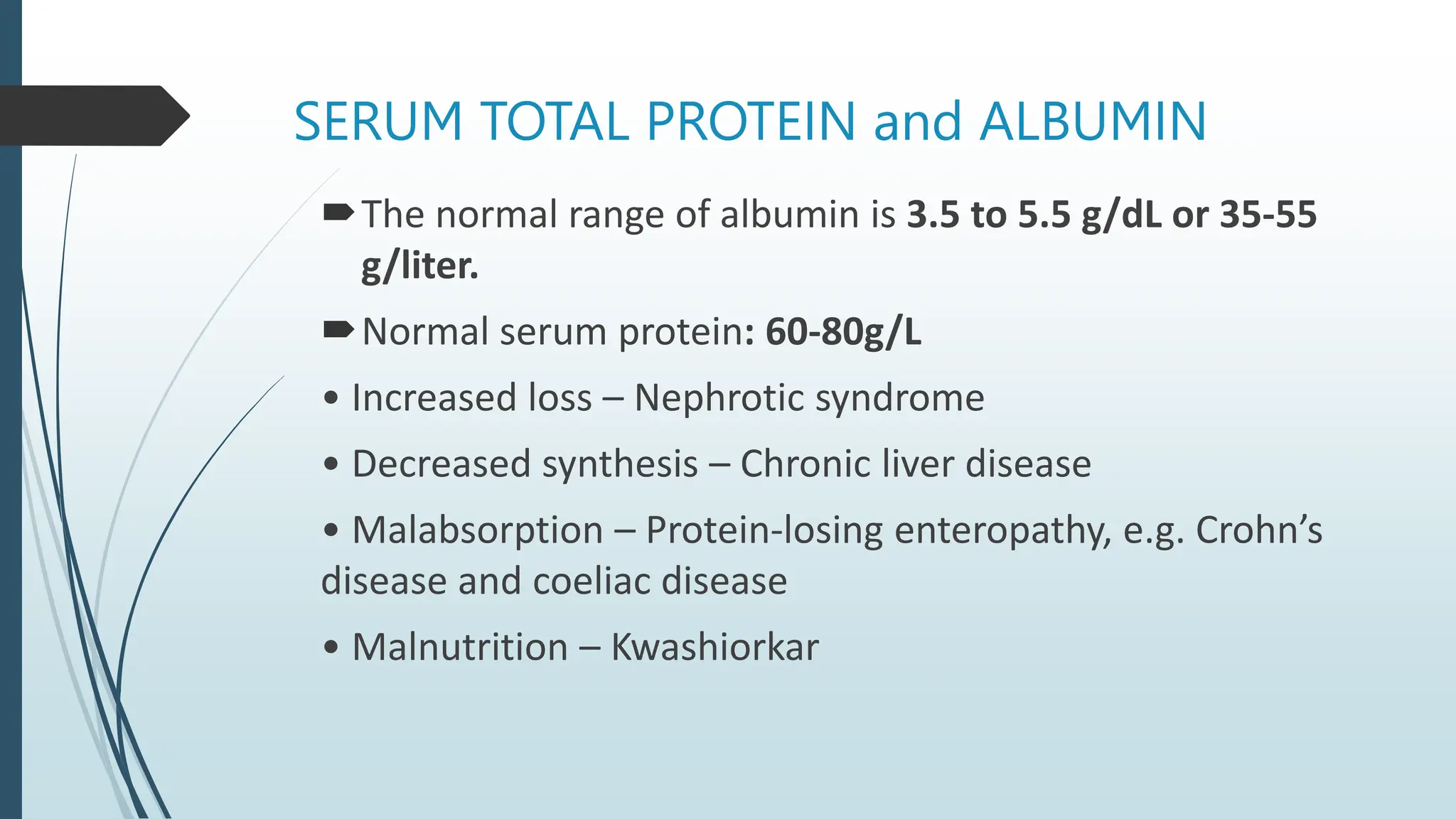
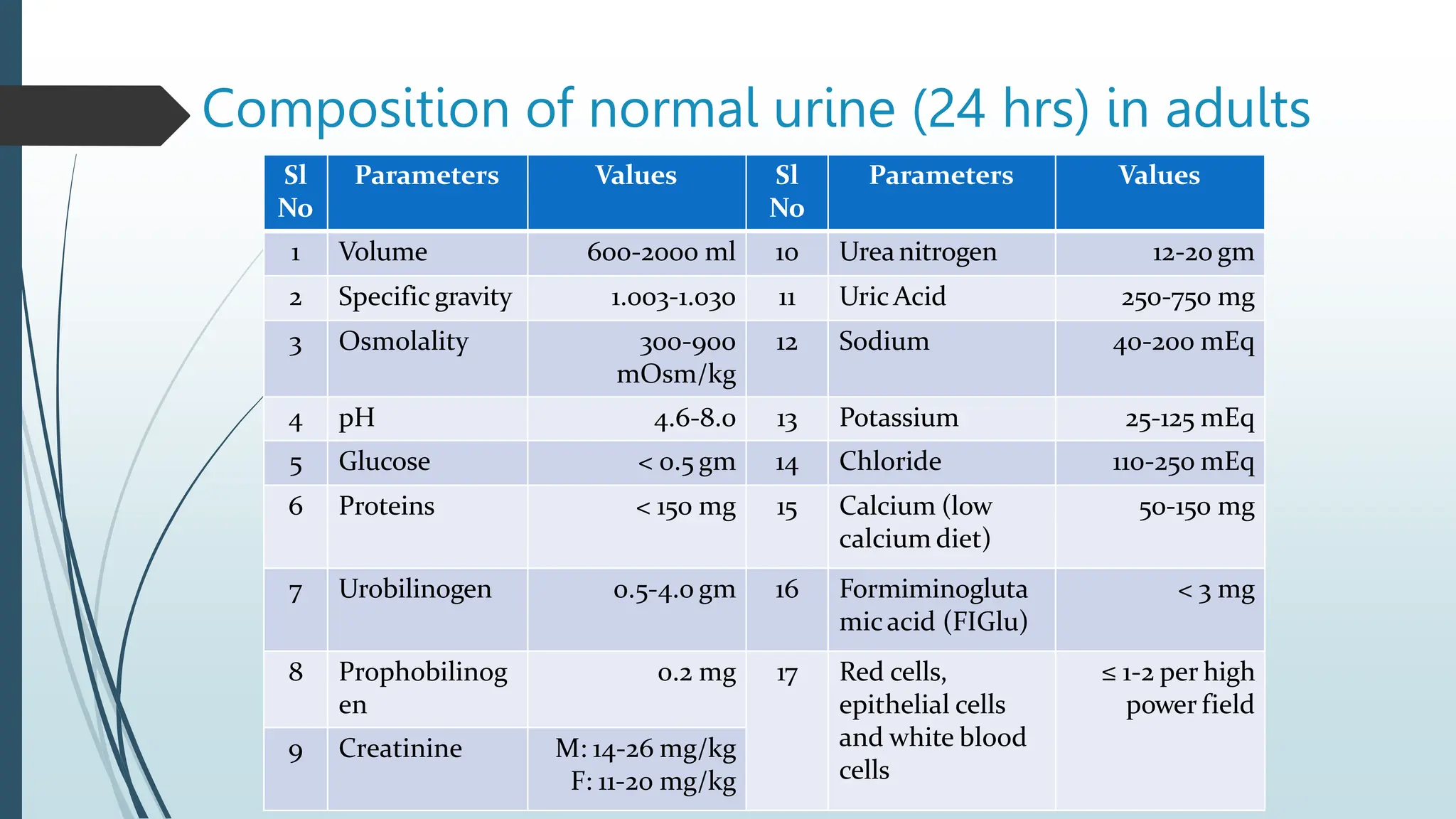
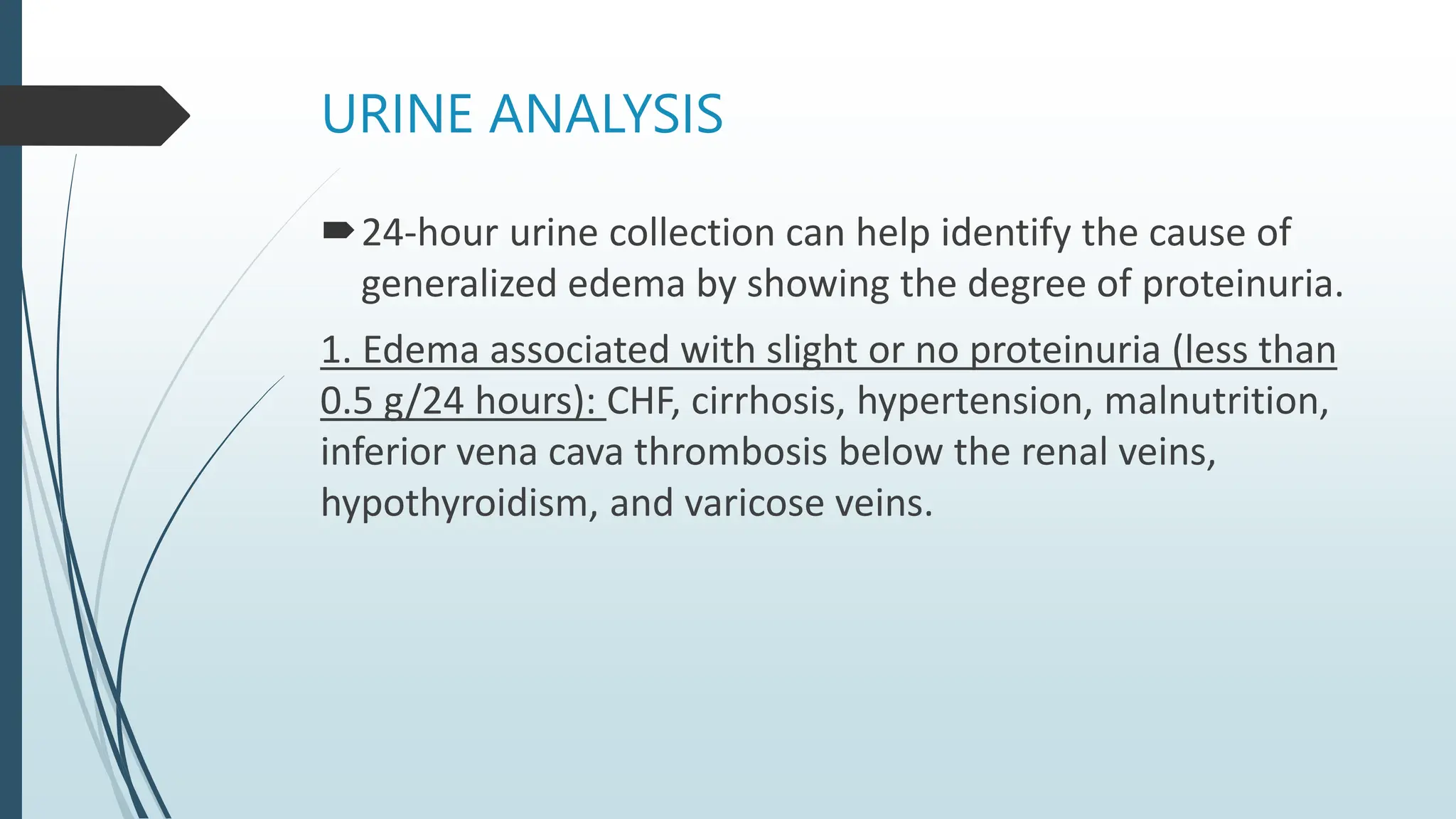
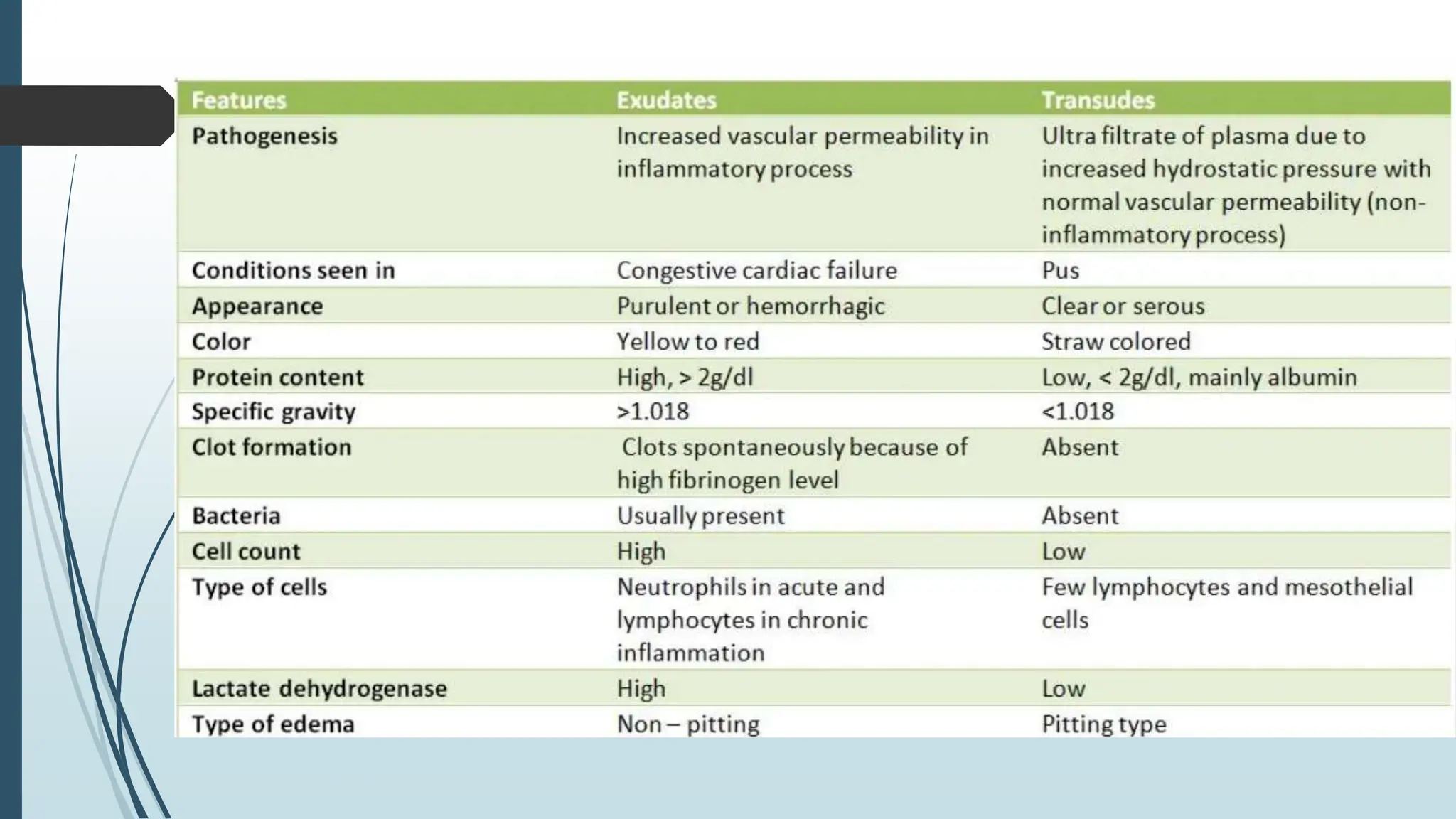
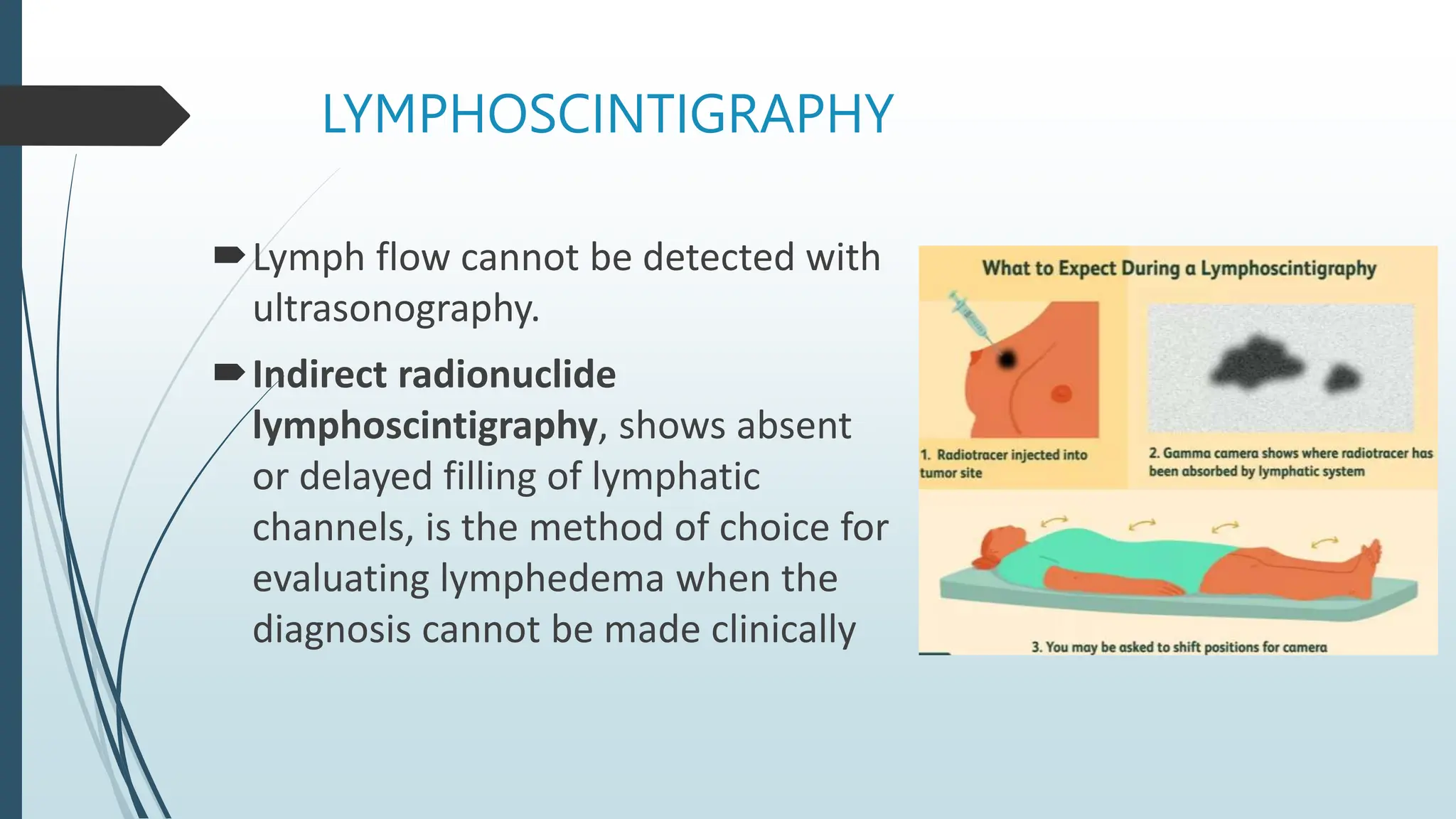
Laboratory investigation of a patient presenting with edema should include tests to identify potential underlying causes. A complete blood count, renal function tests, liver function tests, serum protein and albumin levels, lipid profile, and thyroid function tests can help detect issues like kidney disease, liver disease, malnutrition, or hypothyroidism. Additional tests like chest x-ray, electrocardiogram, brain natriuretic peptide, D-dimer, ultrasound of the abdomen and pelvis, Doppler study, lymphoscintigraphy, and echocardiogram can help diagnose causes such as congestive heart failure, deep vein thrombosis, or lymphatic abnormalities. Together, these lab tests aim to determine the cause and guide treatment of the