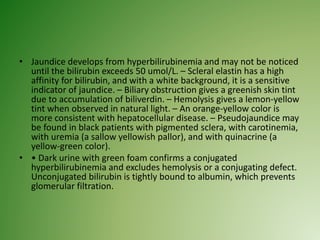
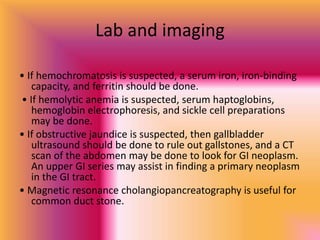
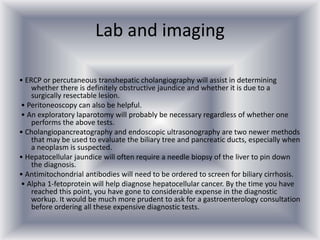
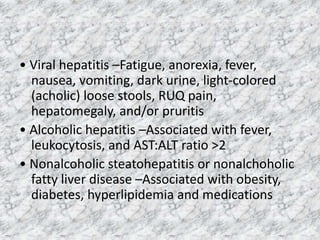
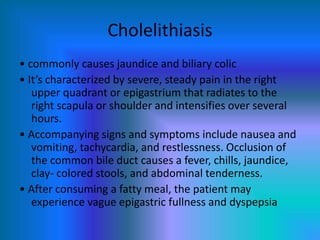
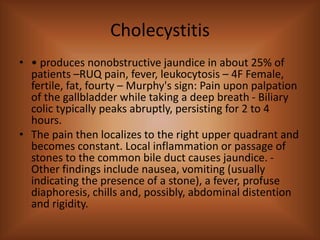
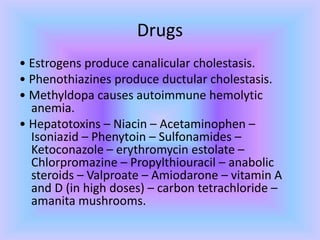
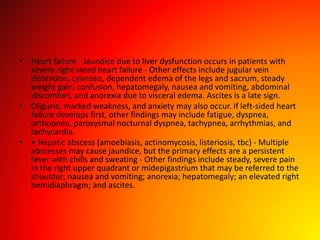
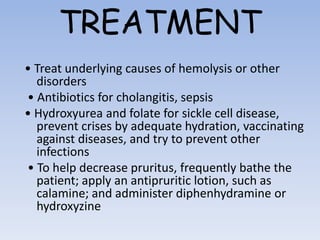
Jaundice, or yellowing of the skin and eyes, is caused by excessive levels of bilirubin in the blood. It can be a sign of liver or bile duct problems. The document discusses the differential diagnosis of jaundice by examining causes related to increased bilirubin production, impaired transport, or decreased excretion. A thorough physical exam and lab work are needed to determine the underlying etiology, such as viral hepatitis, gallstones, drugs, heart failure, or hepatic abscesses. Treatment involves addressing the specific cause and managing symptoms like pruritus.