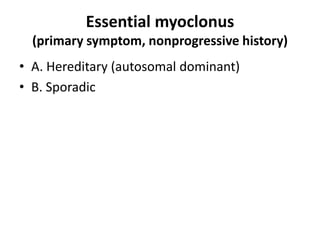
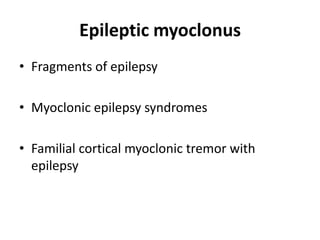
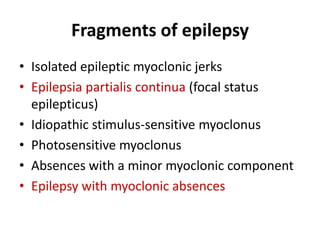
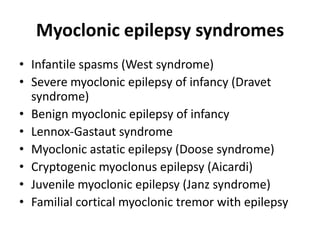
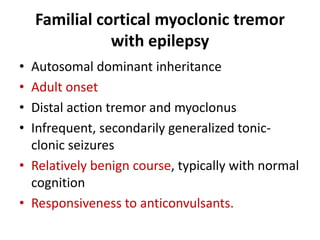
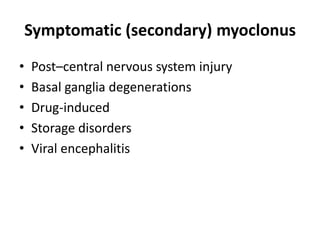
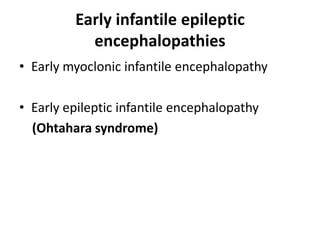
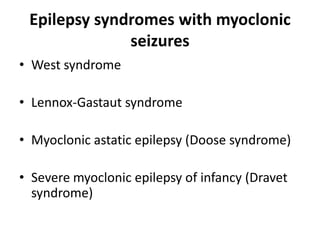
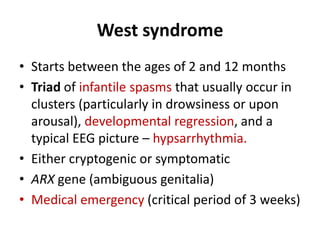
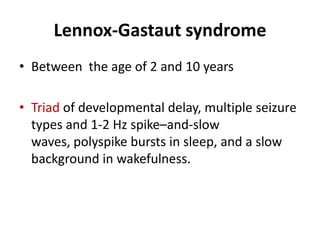
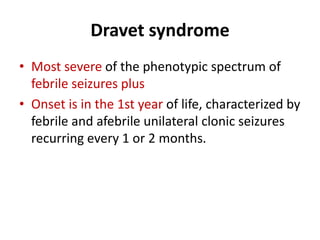
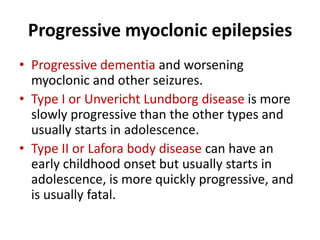
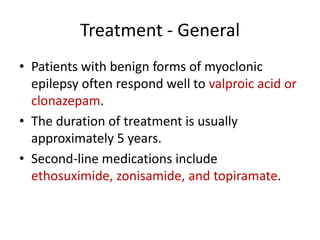
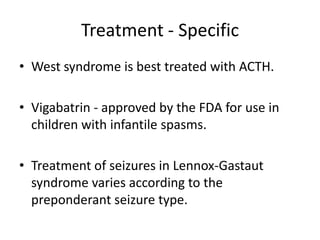
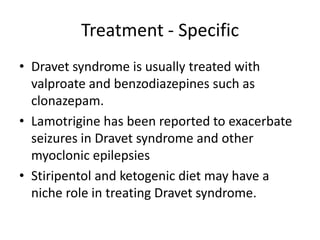
This document discusses the classification and treatment of myoclonic seizures in childhood. It classifies myoclonus into physiological, essential, epileptic, and secondary categories. It describes several epilepsy syndromes that involve myoclonic seizures, including West syndrome, Lennox-Gastaut syndrome, Doose syndrome, and Dravet syndrome. Treatment depends on the specific syndrome but may include valproic acid, clonazepam, vigabatrin, ACTH, a ketogenic diet, and avoiding medications like lamotrigine that can exacerbate seizures.