This document provides information about epilepsy including:
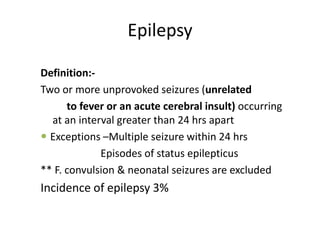
1. It defines epilepsy as two or more unprovoked seizures occurring more than 24 hours apart, with some exceptions. The incidence is about 3% globally.
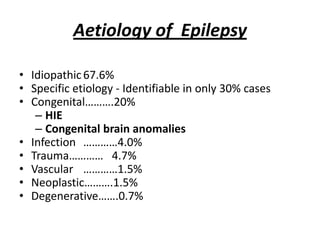
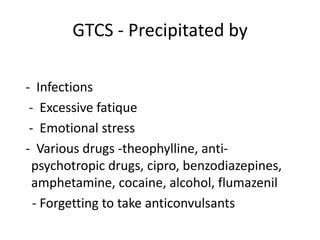
2. It discusses the various causes/aetiologies of epilepsy including idiopathic, congenital, infections, trauma, vascular issues, tumors, and degenerative conditions.
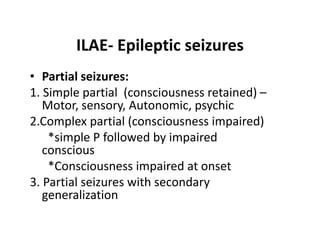
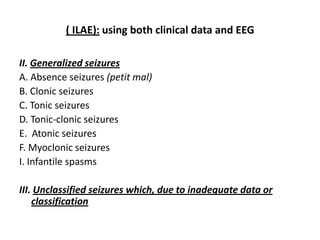
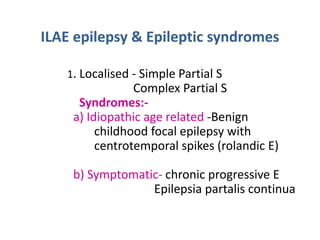
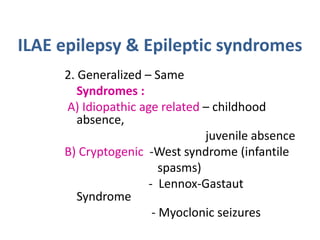
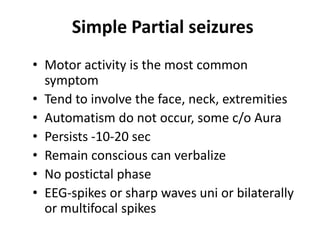
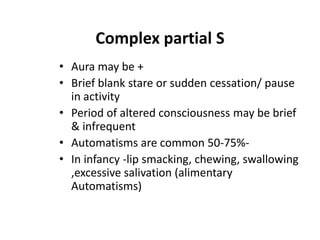
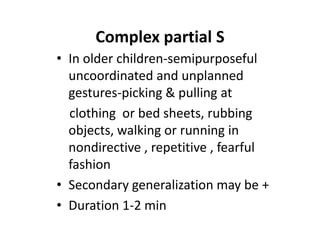
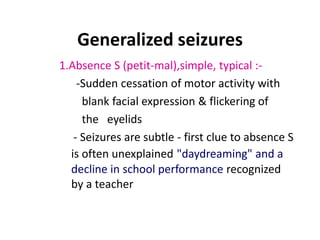
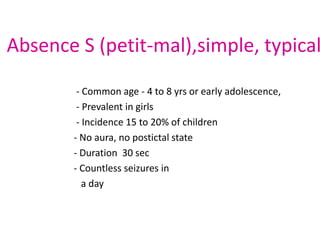
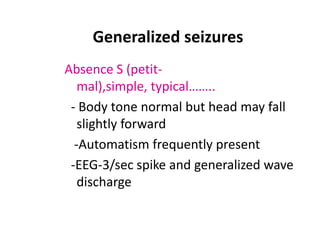
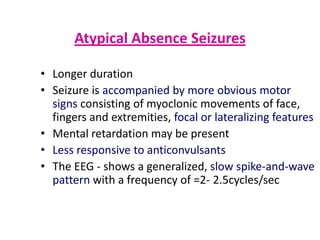
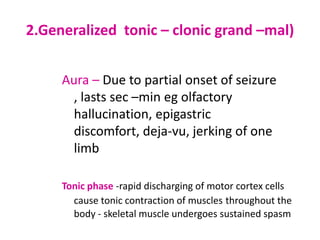
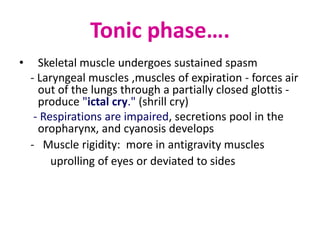
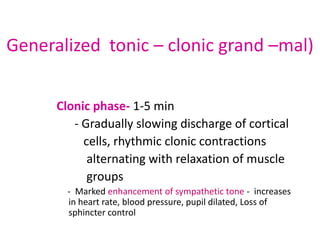
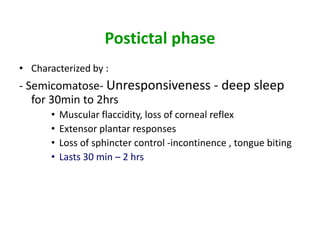
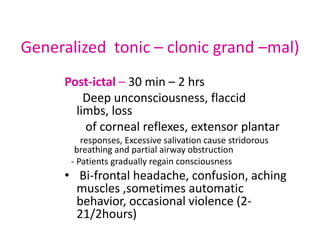
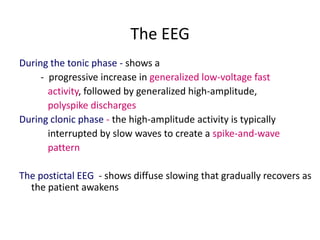
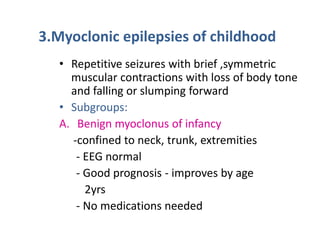
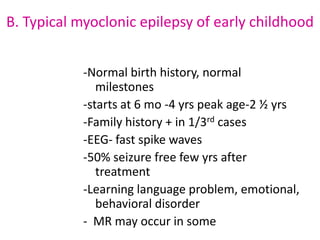
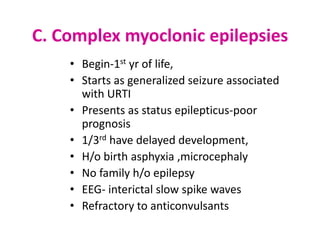
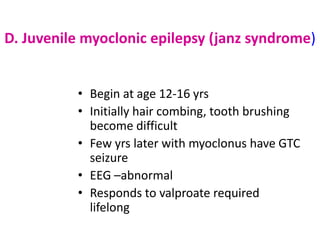
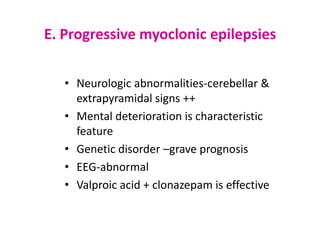
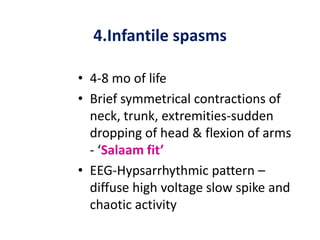
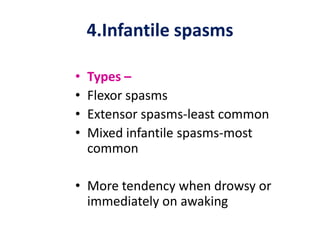
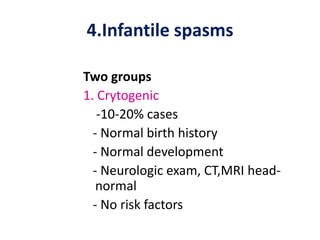
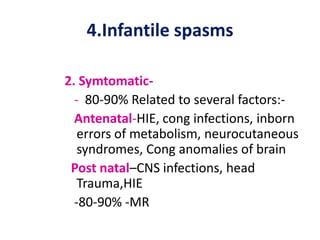
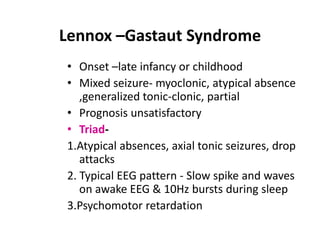
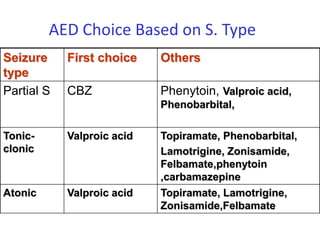
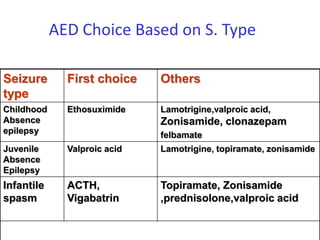
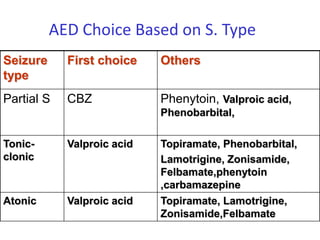
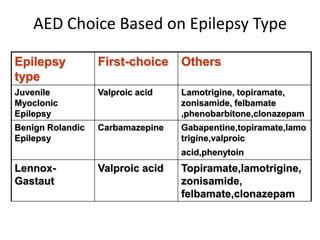
3. It classifies seizure types according to the International League Against Epilepsy including partial seizures, generalized seizures like absence seizures, myoclonic seizures, and infantile spasms.
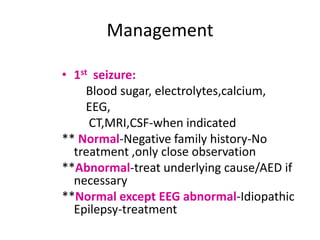
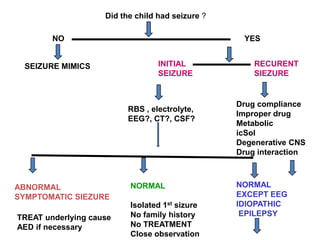
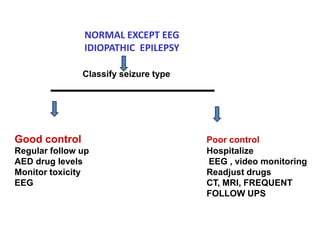
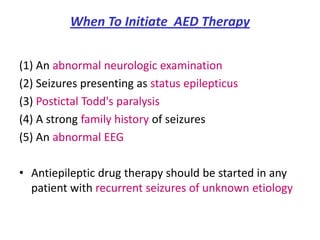
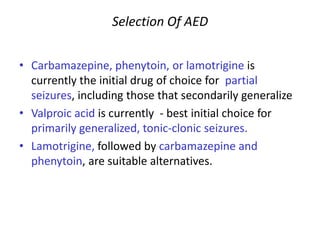
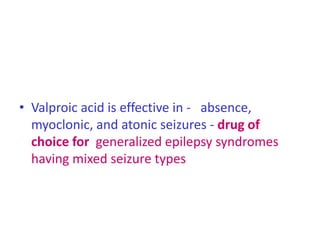
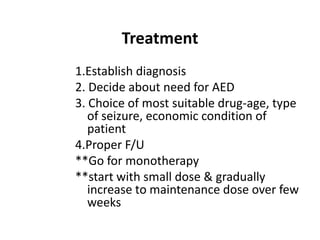
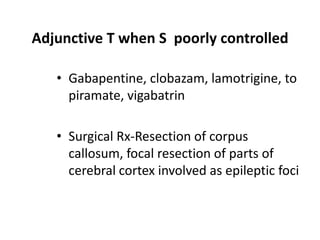
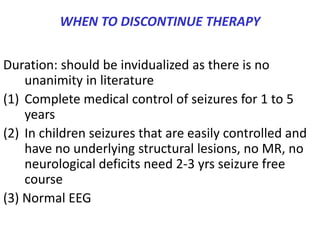
4. It outlines the management of epilepsy including establishing the diagnosis, deciding if antiepileptic drug therapy is
![Epilepsy
Dr. Kalpana Malla
MD Pediatrics
Manipal Teaching Hospital
Download more documents and slide shows on The Medical Post [ www.themedicalpost.net ]](https://image.slidesharecdn.com/cns-epilepsy-120105095406-phpapp02/75/Epilepsy-1-2048.jpg)
![Thank you
Download more documents and slide shows on The Medical Post
[ www.themedicalpost.net ]](https://image.slidesharecdn.com/cns-epilepsy-120105095406-phpapp02/85/Epilepsy-47-320.jpg)