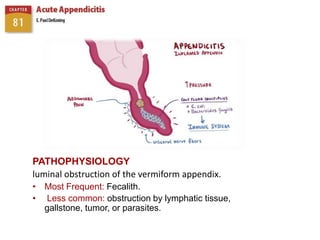
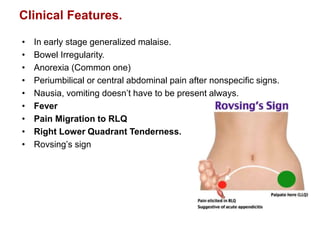
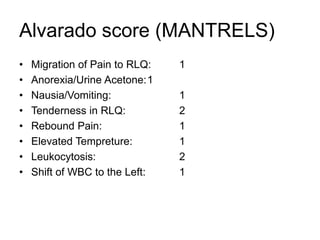
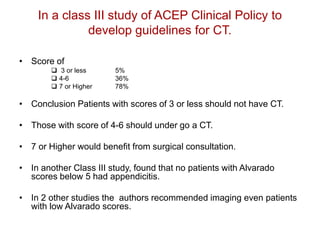
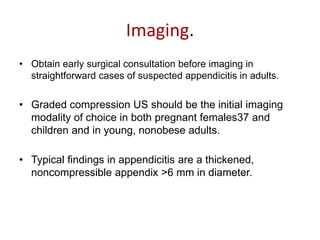
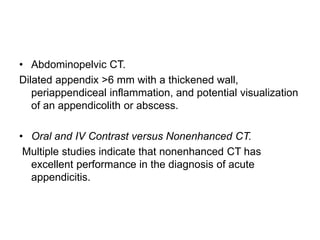
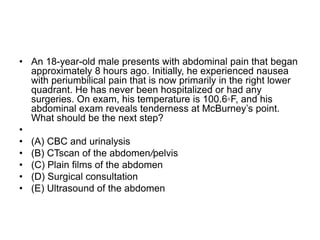
Acute appendicitis is caused by luminal obstruction of the vermiform appendix, most commonly by a fecalith. Clinical features include periumbilical or right lower quadrant pain, anorexia, nausea, and tenderness in the right lower quadrant. The Alvarado score is used to determine the likelihood of appendicitis and need for imaging or surgical consultation. For patients presenting with suspected appendicitis, ultrasound is usually the initial imaging choice, while CT is also effective for diagnosis. Surgery is the standard treatment for confirmed acute appendicitis.