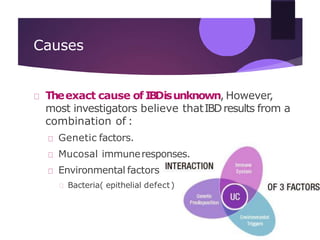
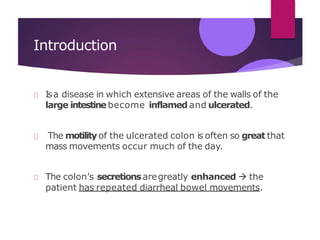
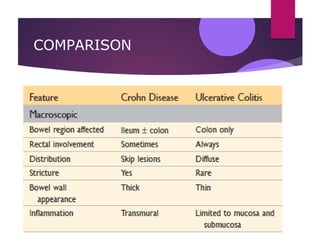
Inflammatory bowel disease (IBD) includes two major entities: Crohn's disease and ulcerative colitis. Crohn's disease can involve any part of the gastrointestinal tract and is transmural, while ulcerative colitis is limited to the colon and mucosa. The exact causes of IBD are unknown but likely involve genetic, immunological, environmental, and bacterial factors. The main differences between the two conditions are the locations they affect and their morphological expression.