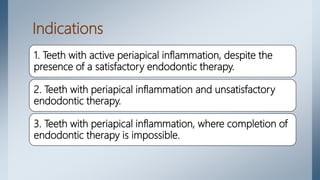
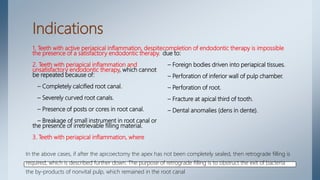
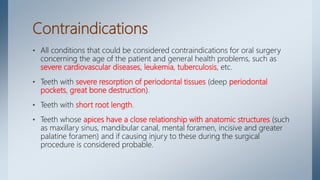
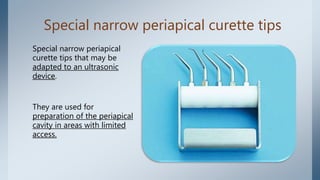
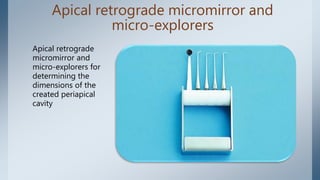
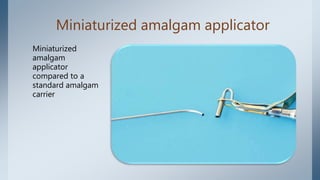
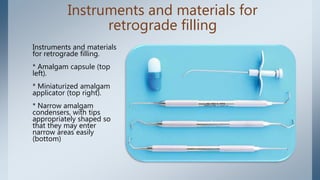
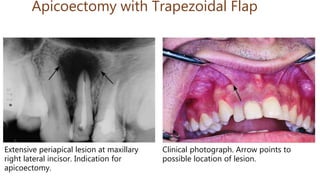
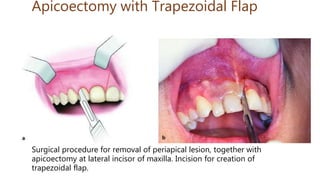
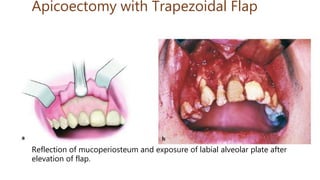
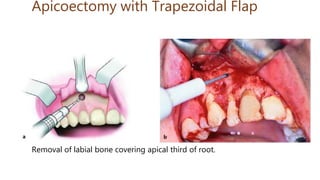
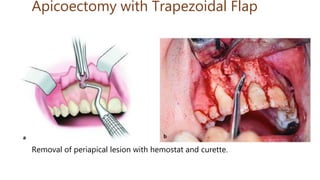
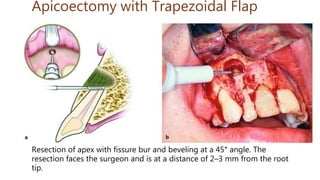
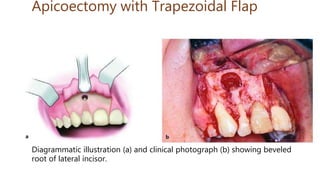
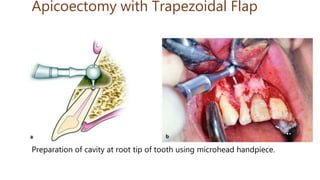
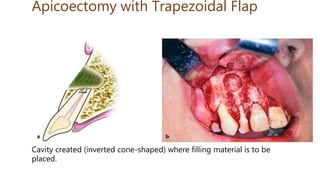
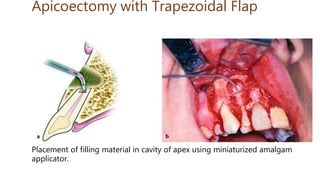
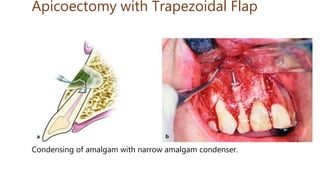
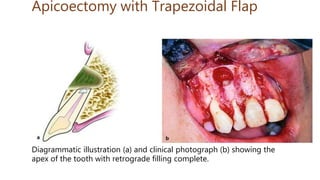
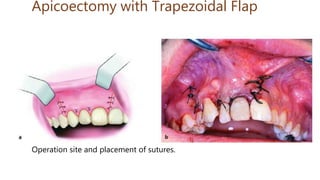
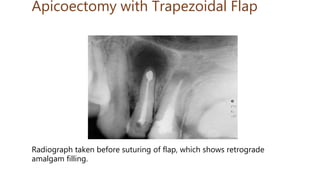
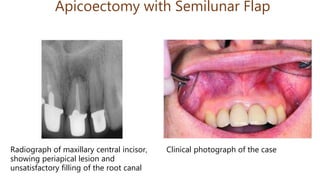
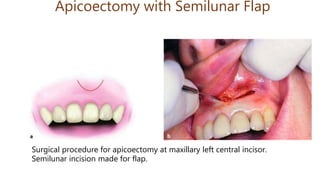
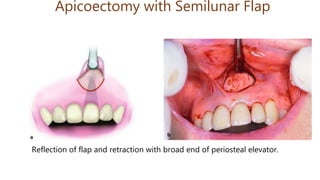
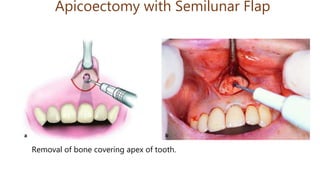
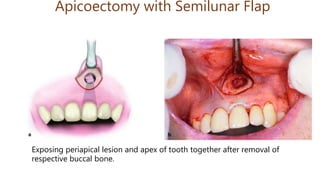
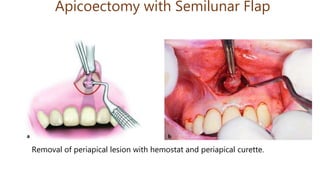
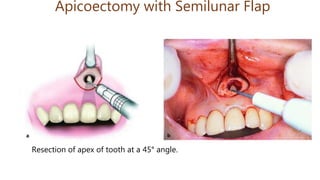
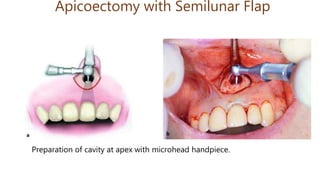
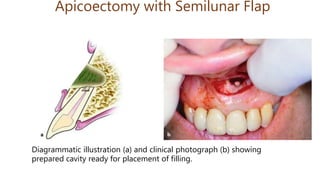
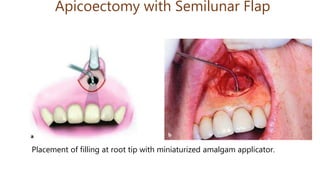
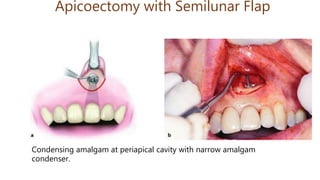
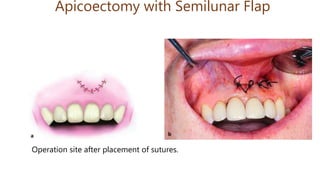
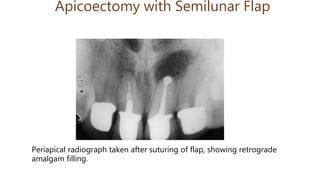
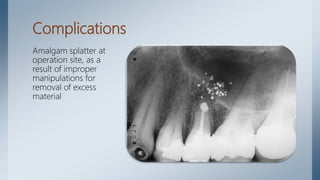
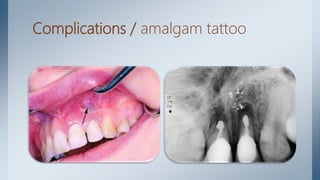
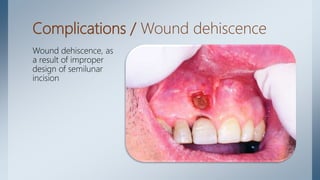
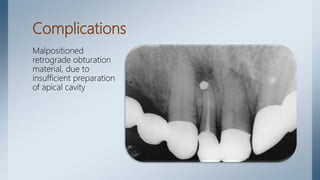
This document provides information about the surgical procedure of apicoectomy. It begins with an introduction defining apicoectomy as the surgical resection and removal of the root tip and pathological periapical tissues. It then lists the indications and contraindications for the procedure. The rest of the document details the armamentarium, surgical technique including designing the flap, localizing and exposing the apex, resection of the apex, retrograde filling if needed, and wound closure. The surgical technique section provides step-by-step details of each part of the procedure.