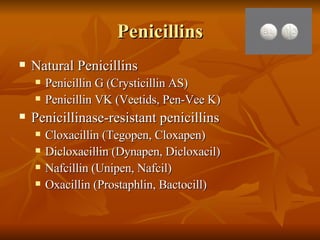
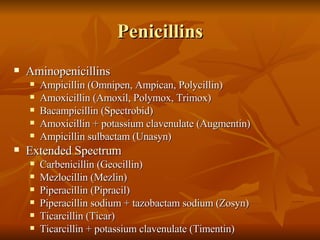
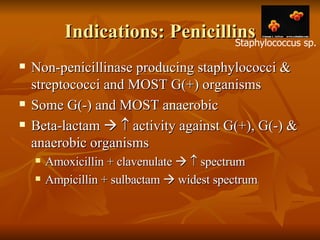
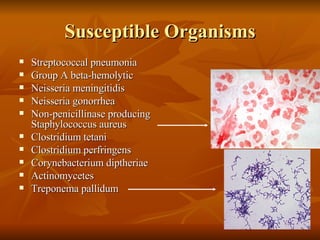
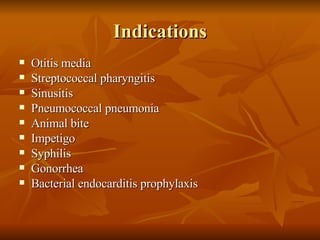
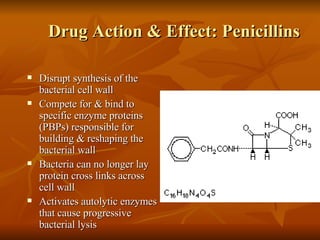
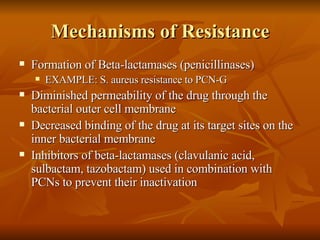
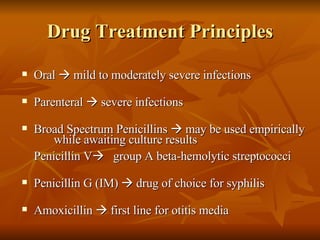
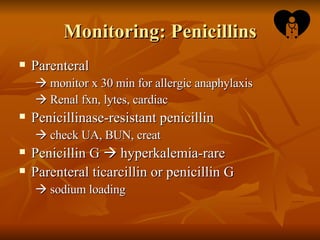
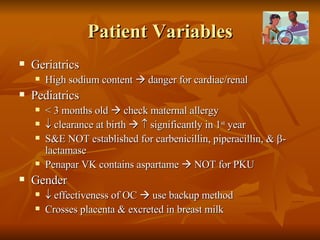
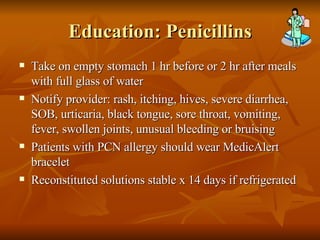
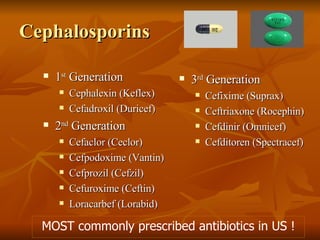
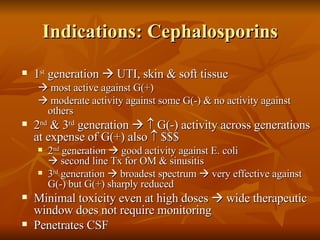
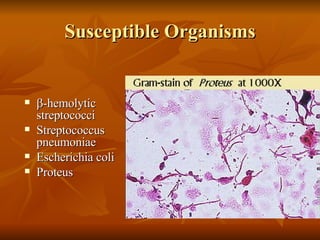
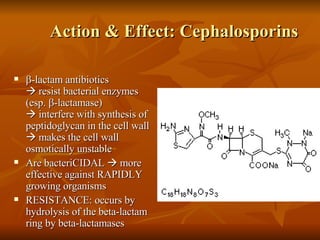
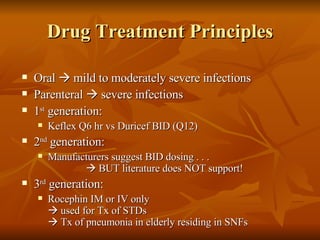
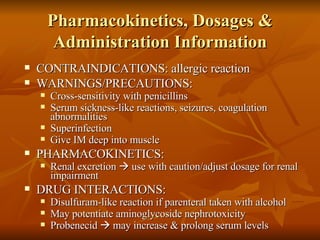
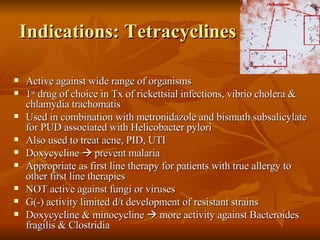
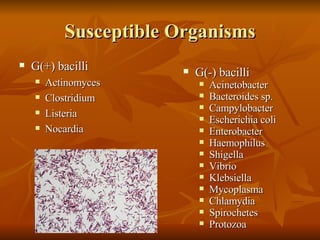
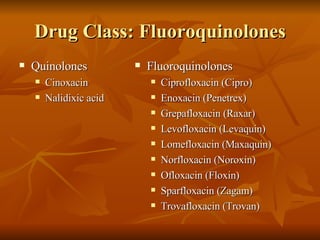
1. The document provides information on various classes of antimicrobial drugs including penicillins, cephalosporins, and tetracyclines.
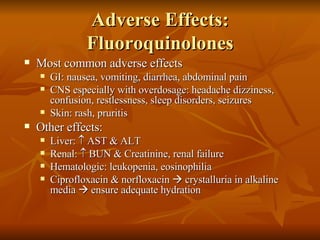
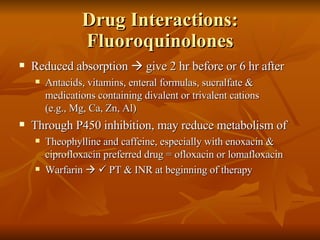
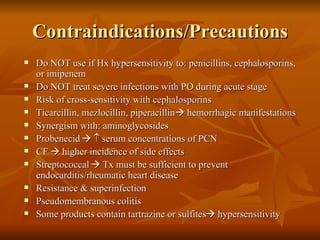
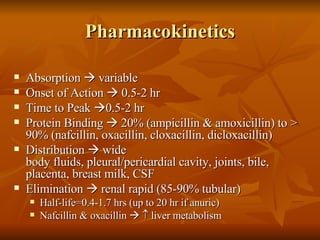
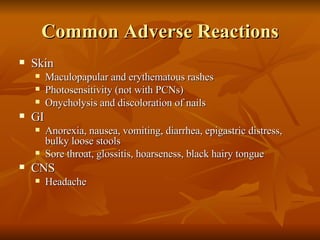
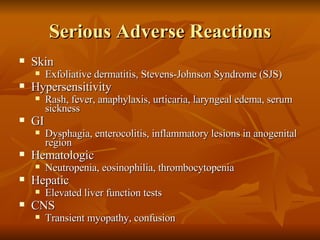
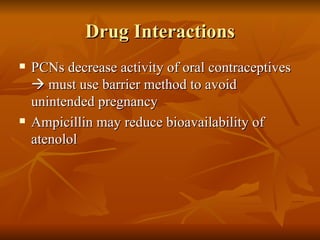
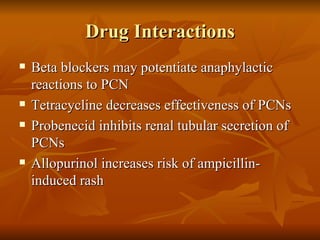
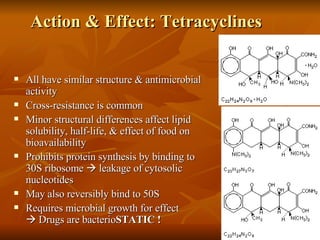
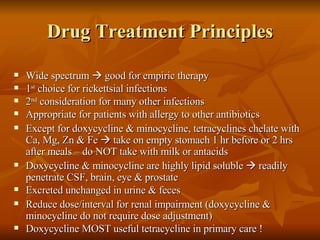
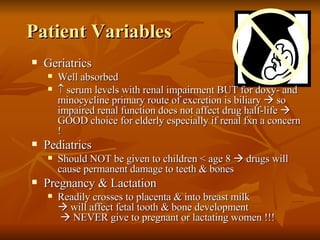
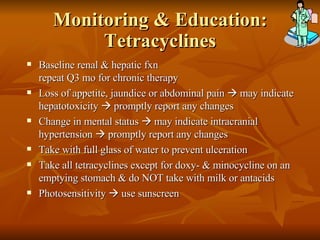
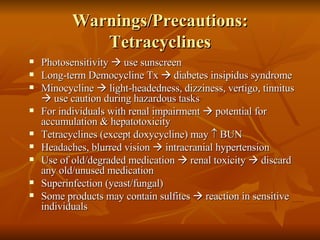
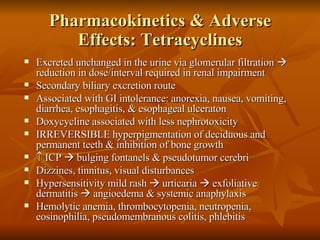
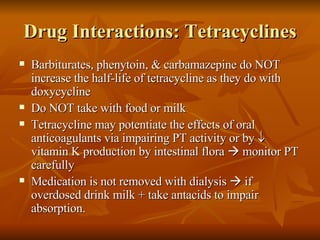
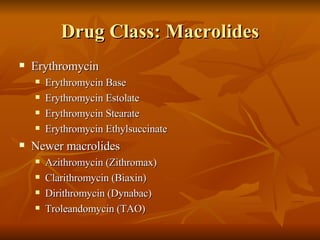
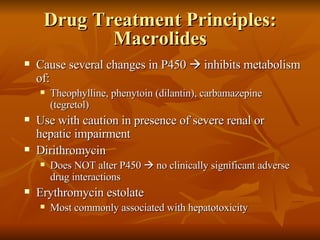
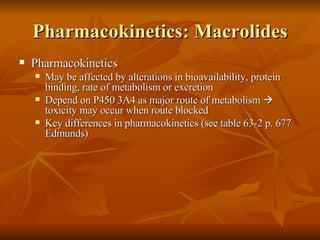
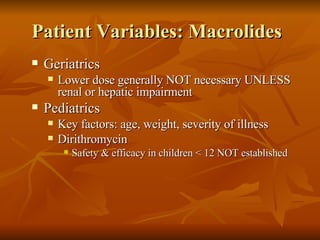
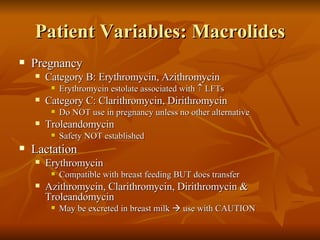
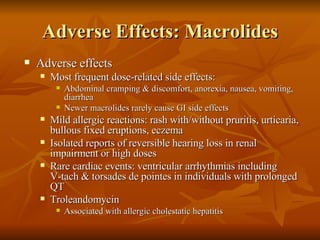
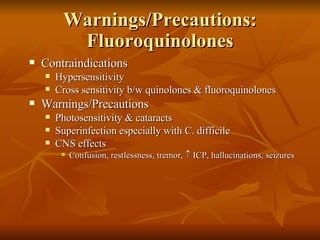
2. It describes the indications, mechanisms of action, drug interactions, and side effects of these commonly used antibiotic classes.
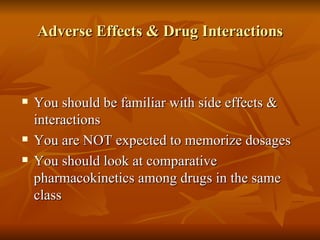
3. The document emphasizes that doctors should be familiar with the side effects and interactions of these drugs when treating patients.

![Pharmacokinetics: Fluoroquinolones Well absorbed after oral administration Widely distributed to most body tissues & fluids High tissue concentrations in: Kidneys, gall bladder, liver, lungs, cervix, endometrium, prostate, & phagocytes High fluid concentrations achieved in Urine, sputum, bile Ciprofloxacin & ofloxacin distributed to Skin, fat, muscle, bone, cartilage, CSF NOT removed by peritoneal or hemodialysis Key differences in pharmacokinetics [seeTable 64-2 p. 683 Edmunds)]](https://image.slidesharecdn.com/antimicrobial2360/85/Antimicrobial-61-320.jpg)